More than 30% of women globally face amenorrhoea, a condition where menstrual periods are absent or irregular. This issue impacts not just reproductive health but also overall well-being. It’s vital to grasp the causes and treatments for amenorrhoea to tackle this common menstrual health problem.
Key Takeaways
- Amenorrhoea is the absence or irregular occurrence of menstrual periods, affecting over 30% of women worldwide.
- The condition can have various causes, including hormonal imbalances, underlying medical conditions, and lifestyle factors.
- Timely diagnosis and appropriate treatment are essential to address amenorrhoea and its potential health implications.
- Both medical and natural therapies can be employed to manage amenorrhoea and restore menstrual regularity.
- Preventive strategies and lifestyle modifications can help reduce the risk of developing amenorrhoea.
What is Amenorrhoea and Its Clinical Significance
Amenorrhoea is when a woman doesn’t get her period. It can affect her health, fertility, and overall well-being. It’s important for both patients and doctors to understand it well.
Primary vs Secondary Amenorrhoea
There are two types of amenorrhoea: primary and secondary. Primary amenorrhoea is when a woman hasn’t had her first period by 16. Secondary amenorrhoea is when a woman who used to have regular periods stops getting them for three months in a row.
Impact on Women’s Health
Amenorrhoea can have a big impact on a woman’s health. It can show signs of ovarian disorders, hormonal imbalances, or serious amenorrhoea diseases. These can cause infertility, osteoporosis, and increase the risk of heart disease if not treated.
It’s key to find and fix the cause of amenorrhoea to keep women healthy and regular.
“Amenorrhoea can be a complex and multifaceted condition, requiring a comprehensive approach to diagnosis and treatment.”
Common Types of Amenorrhoea Diseases
Amenorrhoea means not having menstrual periods. It can be caused by many medical conditions. Knowing the different types is key for the right treatment.
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder. It leads to ovarian disorders and hormonal imbalances. People with PCOS often have irregular or no periods, too much androgen, and cystic ovaries.
Hypothalamic Amenorrhea is another common type. It’s caused by stress, too much exercise, or being too thin. In this case, the brain’s hypothalamus doesn’t send the right signals for the menstrual cycle.
Premature Ovarian Failure (POF) happens when ovaries stop working early. This leads to hormonal imbalances and no periods. It can be caused by genetics, autoimmune diseases, or some medical treatments.
These are just a few examples of ovarian disorders and hormonal imbalances that cause amenorrhoea. Knowing the specific causes helps doctors find the best treatments.
“Amenorrhoea is not a disease in itself, but rather a symptom of an underlying medical condition. By identifying the root cause, healthcare professionals can develop tailored strategies to restore menstrual function and overall reproductive health.”
Hormonal Imbalances Leading to Menstrual Cessation
Menstrual irregularities and hormonal imbalances often go hand in hand. Several hormonal conditions can cause menstrual cessation, leading to amenorrhoea. Let’s explore the key hormonal factors that disrupt the menstrual cycle.
Thyroid Dysfunction
The thyroid gland is key in regulating hormonal balance. Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can affect the menstrual cycle. Hypothyroidism may cause irregular, heavy, or missed periods. Hyperthyroidism can lead to lighter or more frequent periods.
Prolactin Abnormalities
Prolactin is a hormone from the pituitary gland. Elevated levels, known as hyperprolactinemia, can cause menstrual irregularities and amenorrhoea. This condition is often linked to pituitary tumors, medications, or underlying medical conditions.
Estrogen and Progesterone Issues
The balance between estrogen and progesterone is vital for a regular menstrual cycle. Imbalances in these hormones, due to hormonal disorders or external factors, can lead to hormonal imbalances and menstrual disruptions, including amenorrhoea.
| Hormonal Condition | Impact on Menstrual Cycle |
|---|---|
| Hypothyroidism | Irregular, heavy, or missed periods |
| Hyperthyroidism | Lighter or more frequent periods |
| Hyperprolactinemia | Menstrual irregularities and amenorrhoea |
| Estrogen and Progesterone Imbalances | Disruptions in menstrual patterns, including amenorrhoea |
Understanding these hormonal imbalances is key to addressing menstrual irregularities and amenorrhoea. Timely diagnosis and treatment can help restore hormonal balance and alleviate symptoms.
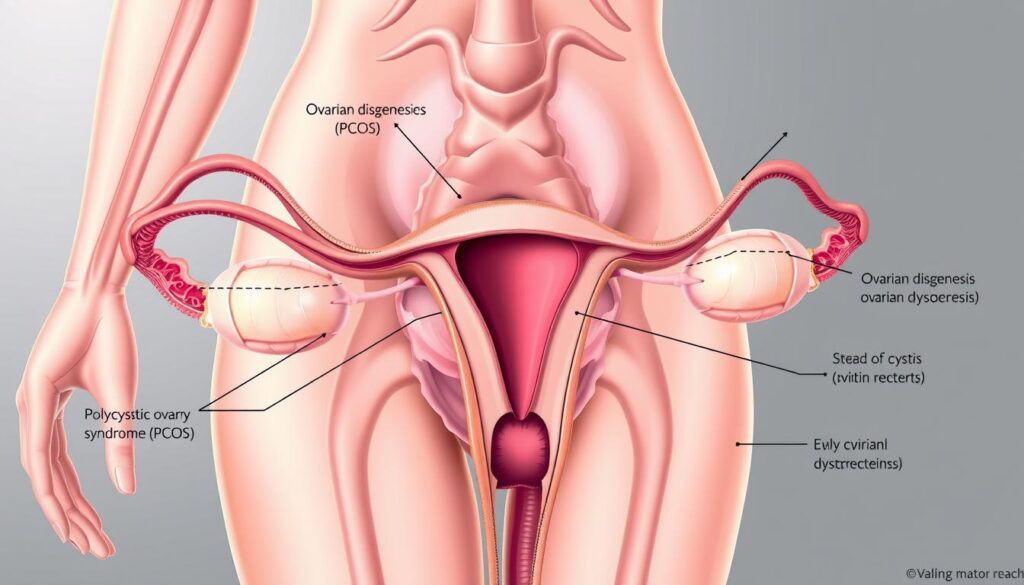
Polycystic Ovary Syndrome (PCOS) and Amenorrhoea
Polycystic Ovary Syndrome (PCOS) is a common hormonal imbalance. It can cause women to miss their periods, leading to amenorrhoea. This condition is marked by multiple small cysts on the ovaries and too much male hormone.
At the heart of PCOS and amenorrhoea is a hormonal imbalance. Women with PCOS have too much luteinizing hormone and too little follicle-stimulating hormone. This stops eggs from being released, causing irregular or no periods.
PCOS can also lead to other health issues. These include polycystic ovaries, infertility, insulin resistance, and a higher risk of type 2 diabetes and heart disease. Understanding PCOS is key to managing it and treating its effects on the menstrual cycle.
“PCOS is a leading cause of amenorrhoea in women of reproductive age, affecting an estimated 5-10% of the female population.”
Diagnosing and Managing PCOS-Related Amenorrhoea
To find the cause of amenorrhoea, doctors do a thorough check. This includes physical exams, blood tests, and imaging. They look for symptoms like irregular periods, too much androgen, and polycystic ovaries.
After diagnosing PCOS-related amenorrhoea, treatment is tailored. It may include lifestyle changes and specific medicines. These aim to balance hormones and get periods back on track.
| Symptom | Prevalence in PCOS |
|---|---|
| Irregular or Absent Menstrual Cycles | 70-90% |
| Excess Androgen Production | 60-80% |
| Polycystic Ovaries | 70-100% |
| Insulin Resistance | 50-70% |
By tackling hormonal imbalances and supporting reproductive health, doctors help women with PCOS. They can get regular periods and improve their life quality.
Understanding Hypothalamic Amenorrhea
Hypothalamic amenorrhea is when you don’t get your period or it’s irregular. It happens because of problems in the hypothalamic-pituitary-ovarian axis. This system controls hormones needed for your menstrual cycle and reproductive health. Knowing what causes hypothalamic amenorrhea is key to fixing it.
Stress-Related Factors
Too much stress can mess with your body’s balance, causing hypothalamic amenorrhea. Stress hormones like cortisol can stop the release of GnRH from the hypothalamus. This leads to a drop in FSH and LH from the pituitary gland. This imbalance can stop your period or make it irregular.
Exercise-Induced Cases
Doing too much exercise, especially if you’re too thin, can also lead to hypothalamic amenorrhea. Hard exercise makes your body think it’s stressed. This causes hormonal changes, including less GnRH, leading to menstrual irregularities or no period at all.
Your body focuses on basic needs over reproductive ones when stressed. This helps save energy but hurts your menstrual health and reproductive chances.

“Hypothalamic amenorrhea is a complex condition that requires a comprehensive understanding of the underlying factors and a multifaceted approach to management.”
Pituitary Gland Disorders and Menstrual Disruption
The pituitary gland is at the brain’s base. It controls many hormones, including those that regulate the menstrual cycle. Problems with this gland can lead to pituitary gland disorders and hormonal imbalances.
Prolactinoma is a common issue. It’s a non-cancerous tumor that makes too much prolactin. This can stop the body from making estrogen and progesterone. This leads to amenorrhea, or no periods at all.
Sheehan’s syndrome happens when the gland is damaged by heavy bleeding or shock after childbirth. This can cause a loss of hormone production, including amenorrhoea.
It’s important to catch and treat these disorders early. This can help restore hormone balance and regular periods. Treatment might include medicine or surgery to remove tumors.
“Pituitary gland disorders can have a significant impact on a woman’s reproductive health, leading to menstrual irregularities and even infertility. Understanding these conditions is key to providing effective management and support.”
By fixing pituitary gland disorders and hormonal imbalances, doctors can help women have healthy menstrual cycles and reproductive health.
Premature Ovarian Failure: Causes and Implications
Premature ovarian failure, or premature ovarian insufficiency, is a serious issue for women’s health. It happens when ovaries stop working early, before 40. This leads to less estrogen and changes in the menstrual cycle. Knowing what causes and affects premature ovarian failure is key to tackling this big health problem.
Genetic Factors
Genetics play a big part in premature ovarian failure. Certain genes, like FMR1, BRCA1, and BPES, raise the risk. Women with a family history of this condition are more likely to get it too.
Autoimmune Conditions
Autoimmune diseases, where the body attacks itself, can also lead to premature ovarian failure. Conditions like Addison’s disease, thyroiditis, and diabetes mellitus can cause this ovarian disorder.
“Premature ovarian failure can have a profound impact on a woman’s fertility, hormonal balance, and overall well-being. Early diagnosis and appropriate management are crucial in addressing this complex reproductive health issue.”
But premature ovarian failure is more than just a fertility issue. Women may also face hot flashes, night sweats, and osteoporosis due to hormonal imbalances. The emotional and psychological effects can be huge, affecting family planning and personal goals.

It’s important to recognize the causes and get medical help early. By understanding the genetic and autoimmune factors, doctors can create treatment plans. This helps each patient and improves their quality of life.
Structural Uterine Abnormalities
When we talk about menstrual issues, looking at uterine abnormalities is key. These changes in the uterus can affect how it works. This can lead to problems like amenorrhoea, where periods don’t come.
Asherman’s syndrome is a condition where scar tissue forms in the uterus. It can happen after certain surgeries. This scar tissue can block the uterus from shedding its lining, causing irregular or missing periods.
There are also congenital uterine anomalies, which people are born with. These can be small changes or more serious issues like a divided uterus. These can mess with menstrual flow, causing irregularities or even no periods at all.
“Structural uterine abnormalities are often overlooked as a potential cause of menstrual irregularities, but addressing these issues can be a critical step in restoring normal menstrual function.”
Healthcare providers need to spot and understand these uterine issues to treat uterine abnormalities and menstrual irregularities. Fixing the problem can help solve symptoms and balance hormones.
Endometriosis and Its Connection to Amenorrhoea
Endometriosis is a chronic condition that affects a woman’s menstrual health deeply. It causes endometrial-like tissue to grow outside the uterus. This can lead to amenorrhoea, or the absence of menstrual periods.
Diagnosis Methods
Finding the cause of amenorrhoea due to endometriosis is hard. Doctors use pelvic exams, imaging tests, and sometimes surgery to diagnose it. Laparoscopy is a surgery that lets doctors see the pelvic organs and find endometrial implants.
Treatment Approaches
Dealing with endometriosis-related amenorrhoea needs a few steps. Hormonal therapy, like birth control pills, can help. In severe cases, surgery might be needed to fix menstrual problems.
Other treatments like acupuncture and herbal remedies can also help. They aim to balance hormones and reduce inflammation. This can help women control their menstrual cycles again.
The link between endometriosis and amenorrhoea shows why early diagnosis and treatment are key. Working with doctors, women can find the best ways to manage this condition. This improves their reproductive health.
Lifestyle Factors Affecting Menstrual Health
Keeping a healthy menstrual cycle is key for women’s health. But, many lifestyle choices can lead to menstrual irregularities and hormonal imbalances. Knowing how these factors affect menstrual health is the first step to solving problems.
Extreme weight loss or obesity can mess with hormone levels. This can cause amenorrhoea (no periods) or irregular periods. Too much exercise, especially for those with low body fat, can also change hormones and affect the menstrual cycle.
Stress, both physical and emotional, plays a big role in menstrual health. Long-term stress can harm the body’s hormone balance. This can lead to hypothalamic amenorrhoea, where the menstrual cycle stops due to stress.
“Stress-induced hormonal changes can directly impact the menstrual cycle, leading to irregular periods or a complete cessation of menstruation.”
What you eat can also affect your menstrual cycle. A diet missing out on nutrients like iron, vitamin B6, and omega-3 fatty acids can cause menstrual irregularities. On the other hand, eating a balanced diet rich in nutrients can help keep hormones in check and support a regular menstrual cycle.
By knowing the lifestyle factors that can impact menstrual health, women can take action. They can work to keep their menstrual cycle regular and healthy. This knowledge helps them make better choices and seek medical help when needed.
Diagnostic Procedures for Amenorrhoea
Identifying the causes of amenorrhoea requires a detailed approach. Doctors use physical exams, lab tests, and imaging to find the problem. This helps them create a treatment plan.
Physical Examinations
The first step is a thorough physical exam. Doctors check the patient’s health and do a pelvic exam. They also look at the patient’s medical history. This gives them a starting point for further tests.
Laboratory Tests
Laboratory tests are key in finding hormonal imbalances. Blood tests check hormone levels like TSH, prolactin, estrogen, and progesterone. These tests help understand why menstruation stopped.
Imaging Studies
Imaging studies are sometimes needed. Tests like ultrasound, MRI, or CT scans help see the reproductive system. They can find problems like uterine or ovarian issues that cause amenorrhoea.
By using these methods, doctors can fully understand the condition. They then create a treatment plan to fix the problem. This helps restore menstrual health and overall well-being.
| Diagnostic Procedure | Purpose |
|---|---|
| Physical Examination | Assess overall health, check for structural abnormalities, review medical history |
| Laboratory Tests | Measure hormone levels (TSH, prolactin, estrogen, progesterone) |
| Imaging Studies | Detect structural issues in reproductive system (ultrasound, MRI, CT scan) |
Healthcare providers use a detailed approach to find the causes of amenorrhoea diseases and ovarian disorders. This leads to treatments that meet each patient’s needs.
Medical Treatment Options
Managing amenorrhoea diseases and hormonal imbalances is key to getting menstrual cycles back. Medical treatments aim to fix the root causes of missed periods. They offer hope to women facing this issue.
Hormone Replacement Therapy
Hormone replacement therapy (HRT) is a main treatment for amenorrhoea. It uses synthetic or natural hormones to balance body levels. This method works well for many types of amenorrhoea caused by hormone or structural issues.
Oral Contraceptives
Oral contraceptives, or birth control pills, are also helpful. They contain hormones that help regulate cycles and bring back normal ovulation. These pills are often used for PCOS or hypothalamic amenorrhoea.
Other Medications
Other meds can also treat amenorrhoea. For example, drugs for thyroid, prolactin, or pituitary issues can help. These address hormonal problems that lead to missed periods.
Choosing the right treatment depends on the person’s situation and the cause of amenorrhoea. A detailed check-up and a tailored plan are crucial. They help manage the condition and improve reproductive health.
Natural and Alternative Therapies
Women dealing with menstrual issues or ovarian disorders can find help in natural and alternative therapies. These methods aim to balance hormones and improve reproductive health. They offer a holistic way to manage these challenges.
Dietary Modifications
Changing your diet can greatly improve menstrual health. Eating foods rich in nutrients that help with hormone balance is key. For example:
- Leafy greens: Full of vitamins and minerals that regulate the menstrual cycle.
- Whole grains: Give complex carbs and fiber for stable blood sugar.
- Lean proteins: Crucial for hormone production and energy balance.
- Healthy fats: In avocados, nuts, and seeds, they support hormone function.
Staying away from processed foods, caffeine, and alcohol can also help. These can worsen menstrual problems and ovarian disorders.
Herbal Remedies
For centuries, herbs have helped with hormonal imbalances and menstrual issues. Some well-known ones are:
- Chasteberry (Vitex agnus-castus): Helps regulate the menstrual cycle and reduces PMS symptoms.
- Black cohosh: Relieves hot flashes and other menopausal symptoms.
- Dong quai: Supports hormonal balance and can help with amenorrhoea.
Always talk to a healthcare professional before trying herbal remedies. They can interact with medications or have side effects.
Natural and alternative therapies give women a holistic way to tackle menstrual irregularities and ovarian disorders. By choosing the right foods and exploring herbs, women can actively work towards better menstrual health and overall well-being.
Prevention Strategies and Risk Factors
Keeping a healthy menstrual cycle is key for women’s health. Understanding the risks and taking steps to prevent them can help. This way, women can manage their reproductive health better and avoid certain issues.
Risk Factors for Amenorrhoea Diseases
- Excessive stress or anxiety
- Significant weight loss or fluctuations
- Intense physical activity or exercise
- Hormonal imbalances, such as thyroid dysfunction or prolactin abnormalities
- Certain medical conditions, including polycystic ovary syndrome (PCOS) and premature ovarian failure
- Structural uterine abnormalities or endometriosis
Prevention Strategies for Menstrual Irregularities
- Manage stress through relaxation techniques, yoga, or meditation
- Maintain a balanced, nutrient-rich diet and a healthy body weight
- Engage in moderate, regular exercise, avoiding excessive or high-intensity workouts
- Consult a healthcare provider for regular check-ups and timely diagnosis of any hormonal or reproductive issues
- Adopt a proactive approach to reproductive health, addressing concerns early on
By knowing the risks and using these prevention tips, women can help keep their menstrual cycles healthy. This approach can lower the chance of amenorrhoea diseases and other menstrual irregularities. Early action and a focus on overall well-being are key to supporting women’s health.
“Menstrual health is a crucial aspect of a woman’s overall well-being, and proactive prevention can make a significant difference in managing amenorrhoea diseases and maintaining regular, healthy menstrual cycles.”
Long-term Health Implications
Amenorrhoea diseases and ovarian disorders can cause long-term health problems. These issues go beyond just missing periods. It’s important for women to know these risks and how to manage them.
One big worry is osteoporosis. Without regular periods, estrogen levels drop. This hormone is key for strong bones. Without it, bones can weaken, raising the risk of fractures.
Also, hormonal imbalances can lead to cardiovascular disease. Amenorrhoea is linked to high blood pressure, bad cholesterol, and insulin problems. These are all heart disease risk factors.
- Decreased bone mineral density and increased fracture risk
- Cardiovascular health concerns, including hypertension and dyslipidemia
- Potential fertility challenges and delayed conception
The impact on fertility is another concern. Missing periods can make it hard to get pregnant. Women with amenorrhoea might face trouble starting a family. They may need special medical help.
| Long-term Health Implications | Risk Level |
|---|---|
| Osteoporosis | High |
| Cardiovascular Disease | Moderate to High |
| Fertility Challenges | Moderate to High |
It’s crucial to tackle amenorrhoea diseases and ovarian disorders early. This can prevent long-term health issues. Regular check-ups, custom treatment plans, and proactive management are key. They help women stay healthy and fertile.
Conclusion
This article has given a detailed look at amenorrhoea diseases. It has talked about their causes, how they affect women’s health, and the treatments available. We’ve seen how hormonal imbalances, menstrual irregularities, lifestyle choices, and physical issues all play a part.
Understanding the hormonal imbalances behind amenorrhoea helps doctors find the right treatment. We’ve looked at conditions like Polycystic Ovary Syndrome (PCOS), hypothalamic amenorrhoea, and premature ovarian failure. This knowledge helps people get the right medical help.
It’s crucial to talk to a doctor for the right diagnosis and treatment of amenorrhoea diseases. By talking openly with healthcare providers, getting the right tests, and trying both medical and natural treatments, people can feel better. This improves their reproductive health and overall well-being.
FAQ
Q: What is amenorrhoea and why is it clinically significant?
A: Amenorrhoea means not having menstrual periods. It’s important because it can show health problems. These include hormonal imbalances and issues with the ovaries or reproductive system. It affects a woman’s health and ability to have children.
Q: What are the different types of amenorrhoea?
A: There are two main types. Primary amenorrhoea is when a woman hasn’t had her period by age 16. Secondary amenorrhoea is when a woman who used to have periods stops getting them for at least 3 months.
Q: What are the common causes of amenorrhoea?
A: Common causes include polycystic ovary syndrome (PCOS) and hypothalamic amenorrhea. Other causes are premature ovarian failure, pituitary gland disorders, and structural uterine problems. Endometriosis is also a cause.
Q: How do hormonal imbalances contribute to amenorrhoea?
A: Hormonal imbalances can disrupt the menstrual cycle. This can happen due to thyroid issues, prolactin problems, or imbalances in estrogen and progesterone. These imbalances can lead to amenorrhoea.
Q: What is the relationship between PCOS and amenorrhoea?
A: PCOS is a common cause of amenorrhoea. It involves hormonal imbalances, including high androgens. This can cause irregular or missing periods.
Q: What is hypothalamic amenorrhea and what causes it?
A: Hypothalamic amenorrhea is caused by a disruption in the hypothalamic-pituitary-ovarian axis. This can be due to stress, too much exercise, or sudden weight loss.
Q: How can pituitary gland disorders lead to amenorrhoea?
A: Pituitary gland disorders, like prolactinoma and Sheehan’s syndrome, can disrupt hormone production. This can lead to irregular periods and amenorrhoea.
Q: What is premature ovarian failure, and how does it contribute to amenorrhoea?
A: Premature ovarian failure is when the ovaries stop working early, before 40. It can cause amenorrhoea and infertility. It’s often linked to genetics or autoimmune conditions.
Q: How do structural uterine abnormalities cause amenorrhoea?
A: Abnormalities like Asherman’s syndrome or congenital uterine anomalies can block menstrual flow. This leads to amenorrhoea.
Q: What is the connection between endometriosis and amenorrhoea?
A: Endometriosis can cause severe pelvic pain and heavy, irregular bleeding. This can lead to amenorrhoea in some cases.
Q: How can lifestyle factors affect menstrual health and contribute to amenorrhoea?
A: Lifestyle factors like extreme weight loss, obesity, too much exercise, and chronic stress can disrupt hormones. This can lead to amenorrhoea.
Q: What diagnostic procedures are used to identify the cause of amenorrhoea?
A: Doctors use physical exams, lab tests, and imaging like ultrasounds or MRI scans. These help find the cause of amenorrhoea.
Q: What are the medical treatment options for amenorrhoea?
A: Treatment options include hormone replacement therapy and oral contraceptives. Medications aim to fix hormonal imbalances or structural problems.
Q: What natural and alternative therapies can help manage amenorrhoea?
A: Natural therapies include dietary changes and herbal remedies. Lifestyle changes like stress management and moderate exercise can also help.
Q: What are the long-term health implications of untreated amenorrhoea?
A: Untreated amenorrhoea can lead to osteoporosis, heart disease, and fertility issues. It’s crucial to seek medical help and follow treatment to manage the condition.
