This condition can really affect someone’s life. It’s a chronic issue that forms near the anus, causing infections, pain, and problems with bowel movements.
It’s important to know what causes it, its symptoms, and how to treat it. This knowledge helps get the right medical care quickly.
Key Takeaways
- Anal fistulas are abnormal, chronic sinus tracts that develop near the anus, often leading to recurrent infections and discomfort.
- Causes of anal fistulas include inflammatory bowel diseases, previous anorectal procedures, and chronic conditions like diabetes.
- Common symptoms include persistent pain, swelling, drainage, and recurrent abscesses around the anus.
- Diagnostic procedures such as endoanal ultrasound and magnetic resonance imaging (MRI) help identify the fistula’s location and complexity.
- Treatment options range from conservative measures to surgical interventions, depending on the individual case and the severity of the condition.
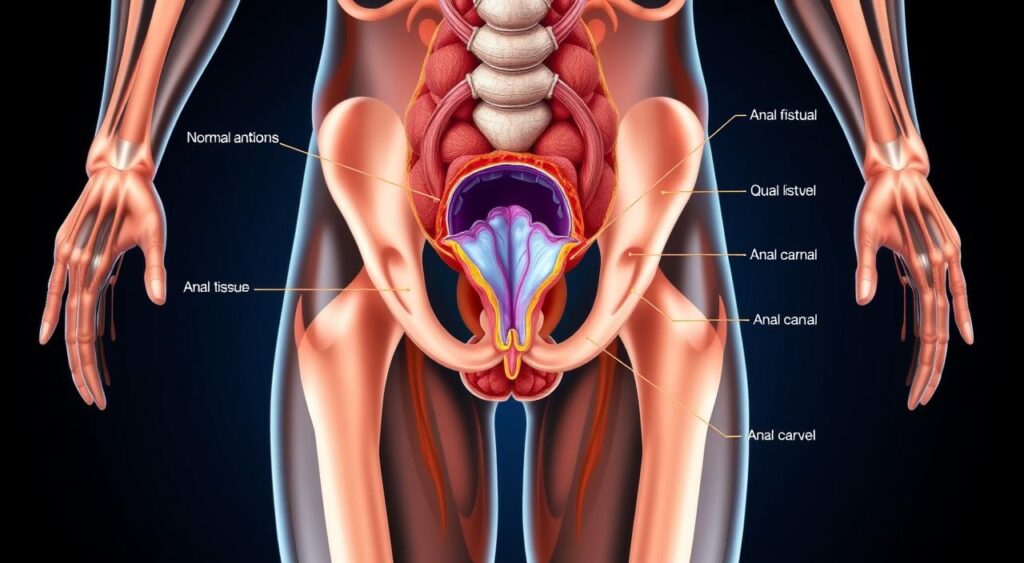
Understanding Anal Fistula: Definition and Overview
An anal fistula is an abnormal tunnel that connects the anus to the skin around it. It often starts from a perianal abscess, a pocket of pus near the anus. This condition can also be linked to pelvic floor dysfunction, affecting the muscles and tissues around the pelvic organs.
Types of Anal Fistulas
Anal fistulas come in different forms. Doctors classify them based on where they start and where they go. The main types are:
- Intersphincteric fistulas: These start inside the anal sphincter muscle and go out through the skin.
- Transsphincteric fistulas: These go through the anal sphincter muscle, linking the rectum to the skin.
- Suprasphincteric fistulas: These go above the anal sphincter muscle before coming out through the skin.
- Extrasphincteric fistulas: These start outside the anal sphincter muscle and connect the rectum to the skin.
Anatomical Structure and Classification
Doctors also classify anal fistulas based on their anatomy and path. They use systems like Park’s classification to describe the fistula’s complexity and location. Knowing the fistula’s anatomy helps in planning the best treatment.
| Classification System | Description |
|---|---|
| Park’s Classification | Categorizes fistulas based on their relationship to the anal sphincter muscles, including intersphincteric, transsphincteric, suprasphincteric, and extrasphincteric types. |
| St. James University Hospital Classification | Focuses on the complexity of the fistula, ranging from simple to complex based on factors such as the number of tracts, presence of abscess, and recurrence. |
| American Gastroenterological Association Classification | Categorizes fistulas as either low (simple) or high (complex) based on their relationship to the anal sphincter muscles. |
Common Causes and Risk Factors
It’s important to know what causes anal fistula to manage and prevent it. This condition can come from infections, inflammatory bowel diseases, and trauma.
Infections and Abscesses
An abscess in the gastrointestinal health area is a main reason for anal fistulas. These abscesses can happen due to bacterial infections like Crohn’s disease or diverticulitis. If not treated, they can turn into fistulous tracts, linking the intestine to the skin.
Inflammatory Bowel Diseases
Crohn’s disease and ulcerative colitis are linked to anal fistulas. These diseases cause inflammation and weaken the anal sphincter. This can lead to fistulous tracts.
Trauma and Previous Surgery
Anal injuries, like those from childbirth or anorectal surgeries, can cause anal fistulas. Such injuries can let bacteria in, creating a fistula.
| Risk Factors | Description |
|---|---|
| Inflammatory Bowel Diseases | Conditions like Crohn’s disease and ulcerative colitis can increase the risk of developing anal fistulas. |
| Diabetes | Individuals with uncontrolled diabetes are more susceptible to developing infections and complications, including anal fistulas. |
| Previous Anal Surgery | Procedures like hemorrhoidectomy or fistulotomy can disrupt the anal anatomy and increase the risk of fistula formation. |
| Radiation Therapy | Radiation treatment in the pelvic or anal region can damage the tissue and increase the likelihood of fistula development. |
Knowing the causes and risk factors of anal fistulas helps healthcare providers. They can then create prevention plans and treatments for those with this anorectal disorder.
Recognizing Anal Fistula Symptoms
Anal fistulas can show different symptoms, ranging from mild to severe. Knowing the main signs and possible complications is key. This helps in getting quick medical help and the right treatment.
Primary Symptoms
The main symptoms of anal fistulas include:
- Persistent pain or discomfort in the anal region
- Drainage or discharge from the fistula opening, which can be pus, blood, or fecal matter
- Swelling or inflammation around the anus
- Difficulty controlling bowel movements or incontinence
Secondary Complications
If not treated, anal fistulas can cause serious problems, such as:
- Recurring perianal abscesses, which are painful pus-filled pockets near the anus
- More anorectal disorders, like extra fistulas or anal fistulas
- Sepsis, a serious condition where the body overreacts to an infection
When to Seek Medical Attention
If you notice any symptoms of an anal fistula, get medical help right away. Early treatment can stop more serious problems and improve your health.
“Prompt diagnosis and proper treatment are vital for managing anal fistulas and avoiding complications.”
By recognizing the signs and getting medical care quickly, people with anal fistulas can take steps to manage their condition. This improves their quality of life.
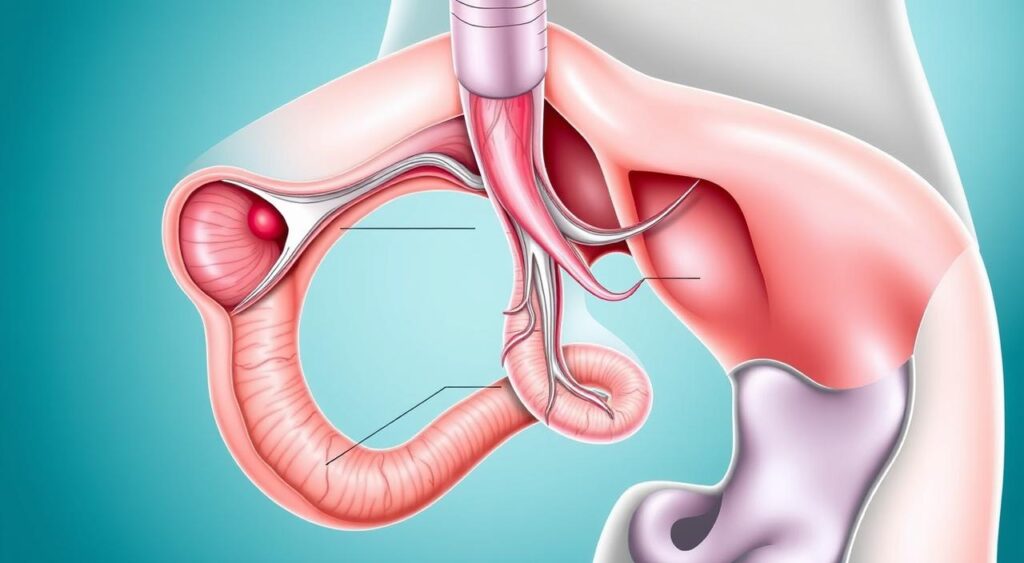
Diagnostic Procedures and Tests
Getting an anal fistula diagnosed right is key to finding the best treatment. Doctors use different tests to figure out the fistula’s details. These tests help them understand where the fistula is, how complex it is, and what might have caused it.
Physical Examination
The first step in finding out about an anal fistula is a detailed check-up. The doctor will look at the anal area and gently touch the affected spot. They’re looking for the fistula’s start and any swelling or abscesses.
Imaging Techniques
Doctors also use imaging tests to learn more about the anal fistula. These include:
- Endoanal ultrasound: This uses sound waves to show detailed pictures of the anal canal and nearby tissues. It helps find out where the fistula is and how complex it is.
- Magnetic Resonance Imaging (MRI): MRI scans give clear images that help doctors plan the fistula surgery and colorectal surgery better.
Specialized Tests
At times, doctors might need more tests to understand the anal fistula better. These might include:
- Fistulogram: This test involves putting contrast dye into the fistula to see its path and any side branches.
- Anorectal manometry: This test checks the pressure and function of the anal sphincter muscles. It helps doctors see how the fistula affects bowel control.
By using these tests together, doctors can fully understand the anal fistula. This lets them create a treatment plan that fits each patient’s needs.
Medical Treatment Options for Anal Fistula
There are many ways to treat anal fistulas. Some treatments are non-surgical, while others involve surgery. Non-surgical methods and medicines can help heal and relieve symptoms.
Conservative Treatment Methods
For mild to moderate fistulas, non-surgical treatments are often used first. These include:
- Sitz baths: Warm, shallow baths that can help reduce inflammation and promote healing.
- Topical ointments: Medicated creams or ointments applied directly to the affected area to reduce swelling and pain.
- Dietary changes: Adjusting your diet to include more fiber-rich foods can help soften stool and prevent further irritation.
Medications and Pain Management
Doctors may also prescribe medicines to help with symptoms. These can include:
- Antibiotics to prevent or treat any underlying infections.
- Anti-inflammatory drugs to reduce swelling and pain.
- Analgesics to provide relief from discomfort and pain.
Preparation for Treatment
Before starting treatment, it’s crucial to work with your doctor. This may involve:
- Undergoing diagnostic tests, such as imaging or endoscopic procedures, to assess the extent and severity of the fistula.
- Making any necessary lifestyle adjustments, such as changes to diet or bowel habits, to support the healing process.
- Discussing any underlying medical conditions or risk factors that may impact the treatment plan.
By understanding the treatment options and working with your healthcare team, you can manage your anorectal disorders better. This improves your gastrointestinal health overall.
Surgical Interventions and Techniques
When anal fistula treatments don’t work, surgery might be needed. Two main surgeries are fistulotomy and the seton technique.
Fistulotomy opens the fistula tract to help it heal. It’s good for simple, low-lying fistulas. This method removes the fistula track and lowers the chance of incontinence.
- The fistulotomy procedure cuts along the fistula to expose it. Then, it’s removed or heals.
- This surgery is usually done as an outpatient under local anesthesia. Recovery takes 2-4 weeks.
The seton technique uses a small thread in the fistula. It slowly cuts through the tissue, healing the fistula from inside.
- This method is for complex or high fistulas. It helps keep the sphincter working and lowers incontinence risk.
- Patients with a seton might need more surgeries, like fistulotomy or fistulectomy, to heal fully.
Choosing between fistulotomy and the seton technique depends on the fistula‘s complexity and location. It also depends on the surgeon’s preference and the patient’s needs. Both surgeries have benefits and risks that need to be talked about with a healthcare provider.
“The goal of surgical treatment for anal fistulas is to eradicate the disease while preserving sphincter function and minimizing the risk of incontinence.”
Recovery and Post-Treatment Care
Recovering from anal fistula treatment is key to managing this health issue. Whether you had conservative treatment or surgery, good care after is vital. It helps with healing, avoids problems, and leads to a better outcome.
Post-Operative Instructions
Your doctor will give you clear instructions after treatment. These include:
- Wound care and dressing changes
- Pain management strategies
- Activity restrictions and physical limitations
- Dietary modifications and fluid intake recommendations
- Medication administration and follow-up appointments
Wound Care Guidelines
Good wound care is essential for healing and avoiding infection. Your healthcare team will give you specific instructions. These may include:
- Keeping the surgical site clean and dry
- Changing dressings as directed
- Avoiding strenuous physical activity or heavy lifting
- Maintaining good hygiene and regular bathing habits
- Seeking immediate medical attention for any signs of complications
| Wound Care Supplies | Purpose |
|---|---|
| Gauze pads | Absorb drainage and protect the surgical site |
| Antiseptic ointment | Prevent infection and promote healing |
| Adhesive bandages | Secure dressings and protect the area |
By following your doctor’s instructions and taking good care of your wound, you can improve your recovery. This reduces the chance of problems linked to fistula treatment, colorectal surgery, and gastrointestinal health.
Prevention Strategies and Lifestyle Changes
Keeping your anal fistula and pelvic floor healthy is key for your gut’s well-being. By using preventive steps and making lifestyle changes, you can lower the chance of getting anal fistulas or having them come back.
One important way to prevent problems is to have good bowel habits. Eating foods high in fiber, drinking plenty of water, and doing Kegel exercises can help. Also, avoid straining when you go to the bathroom and treat any diseases like Crohn’s or ulcerative colitis right away.
Keeping the area around your anus clean and dry is also vital. Use gentle cleansers and avoid things that might irritate your skin. If you notice any signs of an anal fistula, get medical help fast. This is important for quick treatment and to stop the problem from getting worse.
| Prevention Strategies | Lifestyle Changes |
|---|---|
| Maintain a fiber-rich diet Stay hydrated Practice pelvic floor exercises Avoid straining during bowel movements Treat underlying conditions promptly Maintain good anal hygiene | Incorporate regular exercise Manage stress and anxiety Quit smoking and reduce alcohol consumption Seek medical attention for any anal discomfort or changes |
Living a healthy lifestyle also helps keep your anal fistula and pelvic floor in good shape. Regular exercise, managing stress, and avoiding smoking and too much alcohol are all good for your gut health.
“Taking proactive steps to prevent anal fistulas can significantly improve quality of life and reduce the risk of recurrence.”
By using preventive steps and making lifestyle changes, you can take care of your anal fistula and pelvic floor health. This helps your overall gut health too.

Long-term Outlook and Recurrence Risks
People with anal fistulas worry about their future and the chance of it coming back. The outlook can change, but it’s key to keep an eye on things and take action early.
Monitoring and Follow-up Care
Seeing a doctor who knows about anorectal issues is a must for those treated for an anal fistula. This helps catch any new problems or complications early. This includes:
- Regular checks to see how healing is going and if the fistula is coming back
- Tests like endoanal ultrasound or MRI to check the anal sphincter and tissues
- Talking about any ongoing or new symptoms like drainage, pain, or discomfort
Quality of Life Considerations
Anal fistulas can really affect how well someone lives, both when they’re active and later on. Things that might make life harder include:
- Chronic Pain and Discomfort: Ongoing fistulas can cause pain and make daily life tough.
- Emotional Distress: The shame and stigma of anorectal issues can lead to anxiety, depression, and lower self-esteem.
- Lifestyle Limitations: Some activities, like exercise or going out, might be hard or avoided because of the fistula.
Dealing with these issues through medical and mental health support can help people with anal fistulas live better in the long run. It improves their overall well-being.
Knowing what to expect, staying on top of follow-up care, and focusing on quality of life can help. Working with a healthcare team can make recovery better and lower the risk of the fistula coming back.
Conclusion
We’ve learned a lot about anal fistula in this detailed look. We’ve covered what it is, its types, causes, and symptoms. This knowledge helps readers understand this complex condition better.
Getting a correct diagnosis is key for treating fistula effectively. Whether it’s through non-surgical methods or surgery, getting medical advice is crucial. It helps manage the condition and avoid serious problems.
Keeping your gastrointestinal health in check is also important. By making healthy choices and taking preventive steps, you can lower your risk of getting an anal fistula. Being aware and acting on symptoms early can greatly improve your health and life quality.
FAQ
Q: What is an anal fistula?
A: An anal fistula is a tunnel or passageway between the anus and the skin around it. It often starts with an infection or abscess in the anal gland. This creates a small opening or tract that connects the anal canal to the skin.
Q: What are the different types of anal fistulas?
A: There are several types of anal fistulas, based on their location and complexity. Common types include intersphincteric, transsphincteric, suprasphincteric, and extrasphincteric fistulas.
Q: What are the common causes and risk factors for developing an anal fistula?
A: Anal fistulas often come from an infection or abscess in the anal gland. This can be due to Crohn’s disease, ulcerative colitis, or previous surgery. Other risks include trauma, radiation therapy, and certain medical conditions.
Q: What are the primary symptoms of an anal fistula?
A: Symptoms include persistent anal pain, recurrent abscesses, and drainage or discharge from the anus. There’s also a small opening or tract near the anus. Patients may feel discomfort during bowel movements and struggle with personal hygiene.
Q: How are anal fistulas diagnosed?
A: Diagnosis involves a physical exam, imaging tests like endoanal ultrasound or MRI, and sometimes specialized procedures. These methods help identify the fistula’s location, extent, and complexity for treatment planning.
Q: What are the non-surgical treatment options for anal fistulas?
A: Non-surgical treatments include antibiotics, drainage of abscesses, and pain and inflammation management. Sometimes, a seton is placed to keep the fistula tract open and promote drainage.
Q: What are the surgical techniques used to treat anal fistulas?
A: Surgical treatments include fistulotomy (opening and cutting the fistula tract), the seton technique, and more complex procedures like advancement flap repair or LIFT.
Q: What should patients expect during the recovery process after fistula treatment?
A: Patients may experience discomfort, bleeding, or drainage after treatment. Proper wound care, pain management, and follow-up with a healthcare provider are key for a successful recovery.
Q: How can patients prevent the development or recurrence of anal fistulas?
A: Good hygiene, a healthy diet, and regular bowel habits can reduce the risk of anal fistulas. Seeking prompt treatment for abscesses or infections and managing underlying conditions can also help prevent fistula formation or recurrence.
Q: What is the long-term outlook for patients with anal fistulas?
A: The long-term prognosis depends on the cause, fistula complexity, and treatment effectiveness. While some may experience recurrence, regular follow-up care and management can improve outcomes and quality of life.
