Aortic dissection is a serious condition that happens to about 2 people per 100,000 each year. It’s a medical emergency with symptoms that need quick action. It happens when there’s a tear in the aorta’s inner layer, causing blood to flow between layers. This can lead to a rupture.
This article will explain aortic dissection, its causes, symptoms, diagnosis, and treatment. Knowing about aortic dissection and its symptoms is key. It helps people get medical help fast, which can save lives and improve recovery chances.
Key Takeaways
- Aortic dissection is a life-threatening condition that requires immediate medical attention.
- Symptoms of aortic dissection can be severe and may include chest or back pain, shortness of breath, and fainting.
- Early detection and treatment of aortic dissection can significantly improve outcomes and reduce the risk of complications.
- Aortic dissection can be diagnosed using imaging tests such as CT scans and MRI.
- Treatment options for aortic dissection may include surgery, medication, or a combination of both.
- Recognizing the symptoms of aortic dissection and seeking medical help promptly is essential for survival and recovery.
Understanding Aortic Dissection
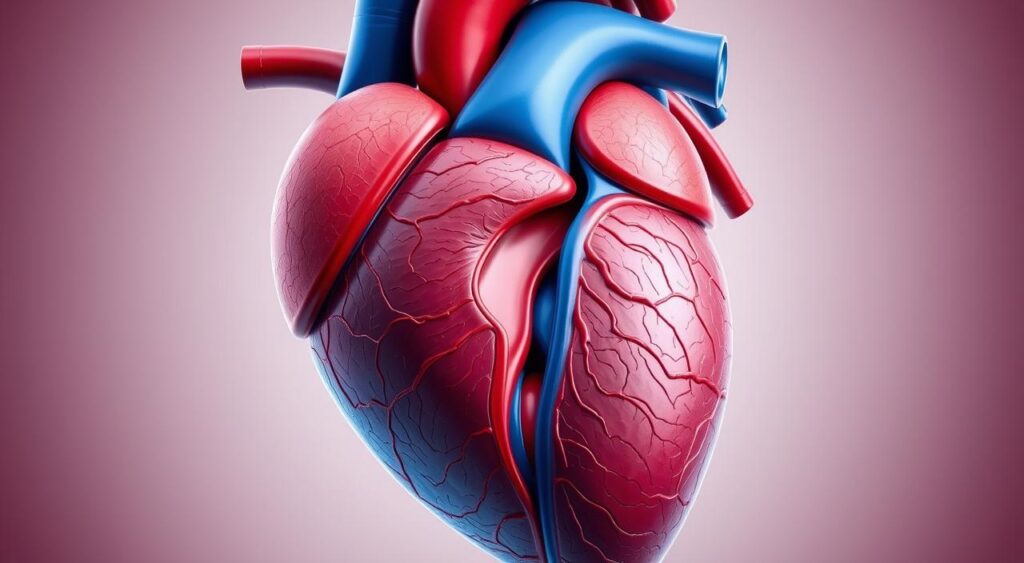
Aortic dissection is a serious condition where a tear happens in the aorta’s inner layer. The aorta is the big blood vessel that comes out of the heart. This tear lets blood flow between the aorta’s layers, causing severe problems.
Definition and Basic Anatomy
The aorta carries blood from the heart to the rest of the body. An aortic dissection happens when the aorta’s wall separates. This creates a false lumen where blood can build up. This separation can make the vessel weak and affect blood flow to important organs.
Types of Aortic Dissection
Aortic dissections are divided into two types:
- Type A: This type affects the ascending aorta and can spread to other parts of the aorta.
- Type B: This type only affects the descending aorta and doesn’t reach the ascending part.
Type A dissections are usually more serious and need immediate surgery. Type B dissections might be treated with medicine and careful watching.
Why It’s a Medical Emergency
An aortic dissection is a medical emergency because of the danger of serious complications. These can include damage to organs, severe blood loss, and aorta rupture. This can lead to sudden death. Quick diagnosis and treatment are key to saving lives and reducing complications.
Common Causes of Aortic Dissection
Aortic dissection happens when the inner layer of the aorta tears. This allows blood to flow between the layers of the aorta’s wall. Knowing the aortic dissection causes is key to preventing and catching it early.
Many things can cause aortic dissection. These weaken the aortic wall, making it more likely to tear. Important aortic dissection causes include:
- Hypertension (High Blood Pressure): Long-term high blood pressure can damage the aortic wall.
- Atherosclerosis: Plaque buildup in arteries can stiffen and weaken the aorta.
- Genetic Conditions: Disorders like Marfan syndrome and Ehlers-Danlos syndrome can affect connective tissue, raising the risk.
- Trauma: Severe chest injuries from accidents can cause aortic dissection.
- Inflammatory Diseases: Conditions such as vasculitis can inflame and weaken the aorta.
Knowing these aortic dissection causes helps people and doctors prevent it. This reduces the risk of this serious condition.
Key Risk Factors You Should Know
It’s important to know about aortic dissection risk factors to prevent and detect it early. Many things can make you more likely to get this serious condition.
Medical Conditions
Chronic high blood pressure is a big risk factor for aortic dissection. It keeps the aortic walls under stress, making them more likely to tear. Also, conditions like Marfan syndrome and Ehlers-Danlos syndrome weaken the aorta, raising the risk.
Lifestyle Factors
Smoking is a big lifestyle risk for aortic dissection. It speeds up atherosclerosis, which can harm the aorta over time. Using stimulants like cocaine also increases the risk by causing sudden blood pressure spikes, which can damage the aorta.
Genetic Predisposition
Genetics also play a part in aortic dissection risk factors. If your family has a history of it, you might be more at risk. This is because inherited weaknesses in the aortic wall can increase your risk. Genetic mutations that affect connective tissue are especially important in raising your risk.
| Category | Risk Factors |
|---|---|
| Medical Conditions | Chronic Hypertension, Connective Tissue Disorders (Marfan, Ehlers-Danlos) |
| Lifestyle Factors | Smoking, Cocaine Use |
| Genetic Predisposition | Family History of Aortic Dissection, Genetic Mutations |
Recognizing the Warning Signs
Early detection of aortic dissection can save lives. Knowing the symptoms of aortic dissection is key for quick medical help.

- Sudden, severe chest or back pain described as tearing or ripping
- Shortness of breath
- Fainting
- Weak pulse
- Differences in pulse between arms
If you notice any of these symptoms of aortic dissection, get help right away. Quick action can greatly improve your chances of recovery.
How Aortic Dissection Is Diagnosed
Getting an accurate diagnosis for aortic dissection is key to effective treatment. Doctors use a detailed process to spot the condition quickly and correctly.
Initial Assessment
The first step is a thorough physical check-up and a detailed medical history. Doctors look for signs like sudden chest or back pain. They also check for risk factors to decide on further tests.
Imaging Tests
Imaging is crucial in diagnosing aortic dissection. Tests like:
- CT Scan: Gives detailed aorta images to spot tears or dissections.
- MRI: Offers clear images without radiation, great for complex cases.
- Echocardiography: Uses ultrasound to see the heart and aorta live.
These tests confirm the dissection’s presence and how far it has spread. They help plan the next steps in treatment.
Laboratory Studies
Blood tests are also used in diagnosis. High D-dimer levels can suggest a dissection. Other biomarkers check overall health and possible complications.
| Diagnostic Method | Purpose | Effectiveness |
|---|---|---|
| CT Scan | Detailed imaging of the aorta | High |
| MRI | High-resolution visualization without radiation | High |
| Echocardiography | Real-time heart and aorta imaging | Moderate |
| Blood Tests | Identify biomarkers like D-dimer | Supporting |
Emergency Treatment Options
Quick aortic dissection treatment is key to saving lives. The first step is to manage pain well to ease the patient’s suffering. Doctors use strong pain relievers for this.
Next, controlling blood pressure is crucial. High blood pressure can make the dissection worse. So, doctors give beta-blockers to lower blood pressure and heart rate.
- Beta-blockers: Reduce heart rate and blood pressure.
- Vasodilators: Help relax blood vessels, lowering blood pressure further.
To stop the dissection from getting worse, doctors closely watch the patient. They might use vasodilators with beta-blockers. In serious cases, surgery is needed right away to fix the aorta and stop it from rupturing.
| Treatment Option | Description | Purpose |
|---|---|---|
| Pain Management | Use of analgesics | Alleviates patient pain |
| Beta-blockers | Medications like esmolol or labetalol | Controls heart rate and blood pressure |
| Vasodilators | Drugs such as nitroprusside | Further reduces blood pressure |
| Immediate Surgery | Open surgery or endovascular repair | Repairs the aorta to prevent rupture |
Surgical Interventions for Aortic Dissection
Aortic dissection surgery is key to keeping patients safe and preventing serious problems. There are two main ways to do this: traditional open surgery and endovascular repair.
Traditional Open Surgery
This method uses a big cut to reach the aorta. It’s often chosen for severe cases needing big repairs. But, it comes with risks like infection, bleeding, and a long recovery.
Endovascular Repair
Endovascular repair is a small incision method. It uses catheters to put a stent graft in the aorta. This way is quicker to recover from and has fewer risks. It’s good for those who can’t handle open surgery.
Post-surgical Care
After surgery, patients need close watching and follow-ups. Recovery includes regular doctor visits, taking medicine, and making lifestyle changes. Following post-surgery advice is key for a good outcome.
Long-term Management and Recovery
After treatment for an aortic dissection, ongoing care is key. Keeping your blood pressure in check is crucial. Your healthcare team will help you manage it safely.
Regular imaging tests are important. They help doctors see how your aorta is doing. This way, they can make any needed changes to your treatment.
It’s important to take your medications as directed. These help control your blood pressure and lower the chance of another dissection.
- Maintain a healthy diet low in sodium
- Engage in regular physical activity as recommended
- Avoid smoking and limit alcohol intake
Making lifestyle changes is also crucial. These can improve your health and help with recovery.
Watching for complications is part of long-term care. Keep in touch with your healthcare team. Tell them about any unusual symptoms right away.
Preventing Aortic Dissection
Preventing aortic dissection starts with taking action. Healthy habits and being alert can greatly lower your risk.
Lifestyle Modifications
Eating well is key to keeping blood pressure and cholesterol in check. Add fruits, veggies, whole grains, and lean meats to your diet. Exercise regularly to boost your heart’s health. And, quitting smoking is crucial to protect your blood vessels and prevent aortic dissection.
Medical Management
Managing your health with medication is important. Use your meds as directed to control blood pressure and cholesterol. Regular doctor visits help keep these conditions under control. Stress management, like meditation or yoga, also plays a role in preventing aortic dissection.
Regular Monitoring
If you have a family history or genetic risk, get checked often. Regular check-ups and scans can spot aortic problems early. Catching issues early means you can act fast, helping prevent aortic dissection.
Life After Aortic Dissection
Surviving an aortic dissection starts a new journey with challenges and hope. It’s important to know about possible complications to live well after recovery.
Patients may face limits on hard activities to avoid more stress on the aorta. Regular health checks are key to watch heart health and catch any issues early.
Emotionally, the recovery can be tough. Many deal with anxiety or depression, making mental health support crucial. Joining support groups helps find a community that understands and supports.
Continuous medical care is key to manage complications. A healthy lifestyle, like a balanced diet and controlled blood pressure, is important for long-term health.
- Chronic pain
- Kidney dysfunction
- Permanent heart damage
- Neurological deficits
| Complication | Management Strategy |
|---|---|
| Chronic Pain | Pain management programs and medications |
| Kidney Dysfunction | Regular renal function tests and appropriate therapies |
| Permanent Heart Damage | Cardiologist consultations and cardiac rehabilitation |
| Neurological Deficits | Neurological assessments and supportive therapies |
Conclusion
Aortic dissection is a serious condition that needs quick action. Knowing its symptoms can save lives by getting medical help fast. New diagnostic tools and treatments have greatly improved survival rates.
Preventing aortic dissection is key. A healthy lifestyle, managing health issues, and regular check-ups are vital. These steps help keep you healthy and lower the risk of future problems.
Knowing about aortic dissection helps you protect your heart. Spotting warning signs and getting help when needed is crucial. By focusing on prevention and regular health checks, you can stay healthy and live longer.
FAQ
Q: What is aortic dissection?
A: Aortic dissection is a serious condition where there’s a tear in the aorta’s inner layer. The aorta is the big blood vessel that comes off the heart. This tear lets blood flow between the aorta’s layers, which can cause a rupture or less blood to vital organs.
Q: What are the symptoms of aortic dissection?
A: Symptoms include sudden, severe chest or back pain that feels like tearing. You might also feel short of breath, faint, or have weakness or numbness in your limbs. A difference in blood pressure between arms is another sign.
Q: What causes aortic dissection?
A: Causes include weakened aortic walls due to high blood pressure, atherosclerosis, and genetic disorders like Marfan syndrome. Traumatic injuries and conditions that stress the aorta also play a role.
Q: What are the risk factors for aortic dissection?
A: Risk factors include high blood pressure, being over 60, and genetic disorders like Marfan or Ehlers-Danlos syndrome. A bicuspid aortic valve, a history of aortic aneurysm, smoking, and cocaine use also increase risk. Family history of aortic disease is another factor.
Q: How is aortic dissection diagnosed?
A: Diagnosis involves a patient’s history, physical exam, and imaging tests. Doctors use CT scans, MRI, or echocardiography to see the aorta. Lab studies help assess the patient’s condition.
Q: What treatments are available for aortic dissection?
A: Treatment depends on the dissection’s type and severity. It often starts with medications to control blood pressure and reduce aorta stress. In severe cases, surgery may be needed to repair the aorta and prevent rupture.
Q: What types of surgery are used to treat aortic dissection?
A: Surgery includes open surgery and endovascular repair. Open surgery replaces the damaged aorta section with a synthetic graft. Endovascular repair uses stent grafts inserted through blood vessels to reinforce the aorta from within.
Q: What are the complications associated with aortic dissection?
A: Complications can be life-threatening, including aorta rupture, organ damage, stroke, heart failure, and death. Long-term issues may include chronic pain, hypertension, and ongoing dissection risk.
Q: How can aortic dissection be prevented?
A: Prevention involves managing risk factors through lifestyle changes. This includes a healthy diet, exercise, avoiding smoking, and controlling blood pressure and cholesterol. Regular monitoring and medical management are key for those with genetic predispositions or existing aortic conditions.
Q: Who is at higher risk for aortic dissection?
A: Higher risk includes those with chronic hypertension, genetic disorders like Marfan syndrome, and a family history of aortic disease. Connective tissue disorders, smoking, and cocaine use also increase risk. Older adults and those with a history of aortic aneurysm are at higher risk too.
Q: What is the recovery process after aortic dissection surgery?
A: Recovery involves hospitalization and rehabilitation. Patients may need to take medications, attend follow-up appointments, and make lifestyle changes. Physical activity is restricted initially, with gradual increase as advised by a healthcare provider.
Q: How does long-term management look after aortic dissection?
A: Long-term management includes ongoing medical care to control blood pressure and regular imaging studies. Lifestyle modifications and adherence to medication regimens are crucial. Patients must also manage any complications and maintain regular follow-ups with their healthcare team.
