Imagine your immune system attacking your liver. This is what happens in autoimmune hepatitis. It’s a condition where the immune system fights the liver, causing damage. It affects about 100,000 to 200,000 people in the U.S.
Autoimmune hepatitis makes the immune system attack the liver’s healthy cells. This leads to inflammation, scarring, and poor liver function. Knowing the causes, symptoms, and getting medical help early are key to managing it.
Key Takeaways
- Autoimmune hepatitis is an autoimmune disorder that causes the immune system to attack the liver, leading to chronic inflammation and potential liver damage.
- The condition affects an estimated 100,000 to 200,000 people in the United States, with a higher prevalence in women.
- Early diagnosis and appropriate treatment are essential to manage the disease and prevent long-term complications, such as cirrhosis and liver failure.
- Treatment typically involves immunosuppressive medications to suppress the overactive immune response and protect the liver.
- Lifestyle changes, including a balanced diet and regular exercise, can also play a crucial role in managing autoimmune hepatitis and maintaining optimal liver health.
Understanding Autoimmune Hepatitis: An Overview
Autoimmune hepatitis is a chronic liver disease. It happens when the immune system attacks and damages liver cells. This condition can take different forms, each with its own characteristics.
Types of Autoimmune Hepatitis
There are two main types of autoimmune hepatitis: type 1 and type 2. Type 1 mainly affects adults, while type 2 is more common in kids and teens. The difference between them is based on the autoantibodies found in the blood.
Role of the Immune System
In autoimmune hepatitis, the immune system goes wrong. It starts attacking the liver’s healthy cells. This leads to inflammation and damage to the liver tissue, affecting its functions.
Impact on Liver Function
As the disease progresses, it can severely damage the liver. This affects its ability to metabolize nutrients, produce proteins, and clear toxins. Liver inflammation and scarring, or cirrhosis, can cause serious problems, like liver failure and an increased risk of liver cancer.
It’s important to understand autoimmune hepatitis. Knowing its subtypes, the immune system’s role, and its effects on the liver is key to managing and treating this complex disease.
“Autoimmune hepatitis is a chronic, progressive liver disease that can lead to cirrhosis and liver failure if left untreated.”
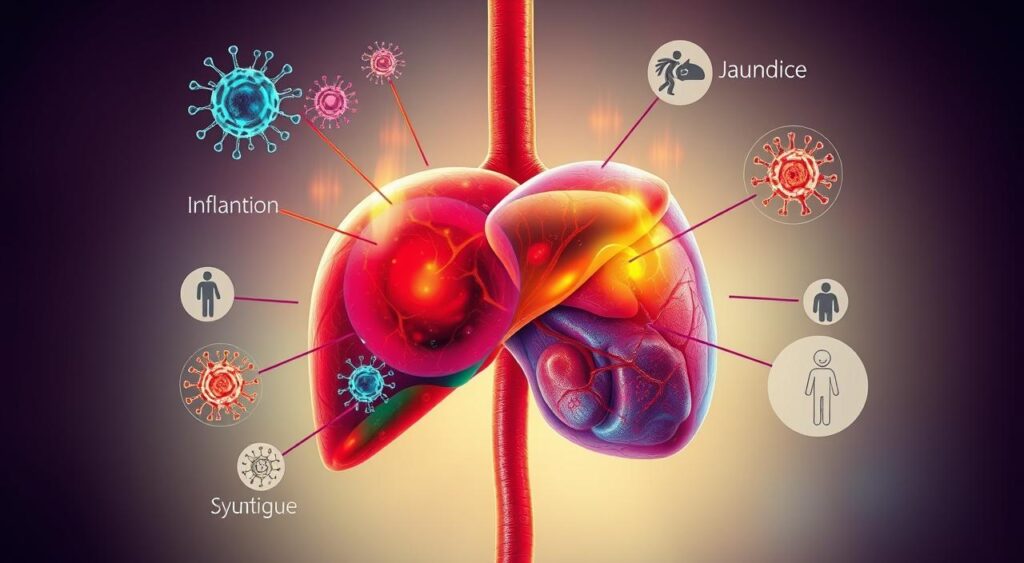
Common Signs and Symptoms of Liver Inflammation
Autoimmune hepatitis is an autoimmune disorder that causes liver inflammation and damage. It’s important to know the signs and symptoms early for proper treatment. People with this condition may feel tired, have yellow skin, and feel pain in their abdomen.
Fatigue is a common symptom. People with autoimmune hepatitis often feel very tired, even after resting well. This is because their body’s immune system is fighting the liver inflammation.
Jaudice is another sign, where the skin and eyes turn yellow. This happens when the liver can’t process bilirubin properly, leading to its buildup.
Abdominal pain is also common. It feels like a dull ache in the upper right part of the belly. This pain comes from the liver’s inflammation and swelling.
Some people with autoimmune hepatitis also have joint pain or arthritis-like symptoms. These problems are related to the body’s immune response and the inflammation it causes.
Knowing these symptoms helps doctors give the right care to patients with autoimmune hepatitis. This can greatly improve their health and quality of life.
| Symptom | Description |
|---|---|
| Fatigue | Excessive tiredness due to the body’s immune system fighting inflammation |
| Jaundice | Yellowing of the skin and whites of the eyes caused by buildup of bilirubin |
| Abdominal Pain | Dull, aching pain in the upper right part of the abdomen |
| Joint Pain | Arthritis-like symptoms due to the autoimmune response and inflammation |
Risk Factors and Genetic Predisposition
Autoimmune hepatitis and chronic hepatitis are complex conditions. They are influenced by many factors. Knowing the risk factors and genetic predisposition is key for early detection and effective management.
Gender and Age Considerations
Autoimmune hepatitis is more common in women, with a female-to-male ratio of about 3.6 to 1. It can happen at any age but is often seen between 40 and 60. Even children can get it, making it important to watch liver health in all ages.
Family History and Genetic Markers
Genetics play a big role in autoimmune hepatitis and chronic hepatitis. People with a family history of these conditions are at higher risk. Certain genetic markers, like specific HLA alleles, increase the risk of autoimmune hepatitis.
Environmental Triggers
Environmental factors also play a part. Certain infections, medications, or toxins can trigger an autoimmune response. This leads to liver inflammation and damage. Knowing and avoiding these triggers can help prevent disease progression.
| Risk Factor | Prevalence | Impact on Disease |
|---|---|---|
| Gender (female) | 3.6:1 female-to-male ratio | Increased risk of developing autoimmune hepatitis |
| Age (40-60 years) | Most common age range for diagnosis | Higher incidence of autoimmune hepatitis in middle-aged individuals |
| Family History | Increased risk in individuals with affected relatives | Genetic predisposition plays a significant role in disease development |
| Environmental Triggers | Varies based on specific exposures | Potential to trigger autoimmune response and liver inflammation |
Understanding these risk factors and genetic predispositions helps healthcare professionals tailor care. Early intervention and proactive management are crucial for maintaining liver health and improving outcomes.
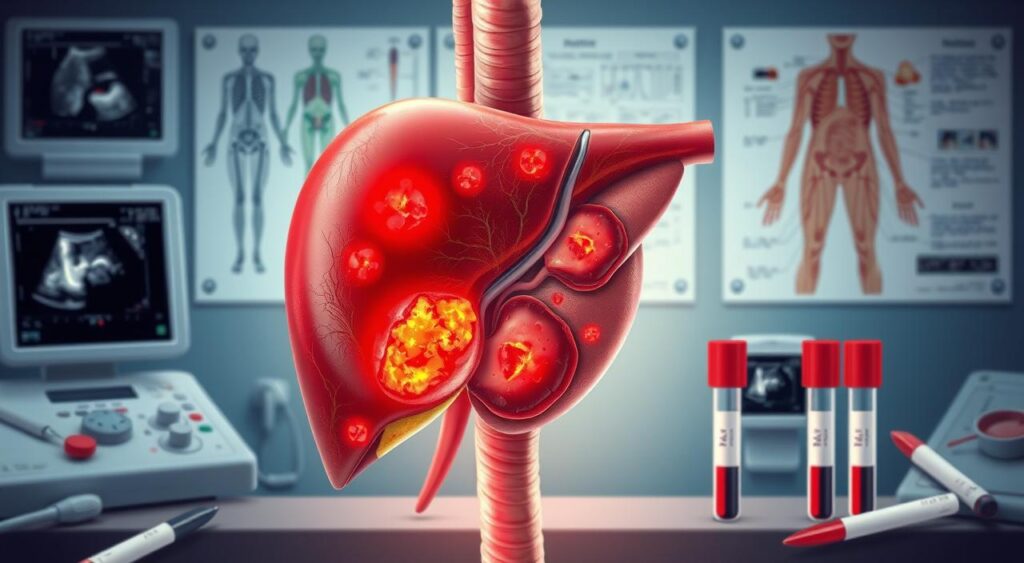
Diagnosing Autoimmune Liver Disease
Diagnosing autoimmune liver disease, like autoimmune hepatitis, needs a detailed check-up by doctors. This includes blood tests, imaging studies, and sometimes a liver biopsy. These steps help find out why the liver is inflamed and not working right.
Checking liver enzymes and autoantibodies in the blood is key. These tests show how much damage the liver has and if it’s an autoimmune issue.
Doctors might also use imaging like ultrasound, CT scans, or MRI to look at the liver. These tools help spot any liver problems or changes.
At times, a liver biopsy is needed to confirm the diagnosis. This involves taking a small liver sample for a closer look. It helps figure out the exact liver disease and how much damage there is.
| Diagnostic Approach | Significance |
|---|---|
| Blood Tests | Assess liver enzymes and autoantibodies to identify autoimmune mechanisms |
| Imaging Studies | Evaluate the structure and function of the liver, detect any abnormalities |
| Liver Biopsy | Confirm the diagnosis and determine the extent of liver damage |
Getting the right diagnosis is vital for treating autoimmune liver disease well. Doctors use different tests to understand the patient’s condition fully. Then, they can create a treatment plan that works best.
“Early and accurate diagnosis is essential for effective management of autoimmune liver diseases, as it allows for timely interventions and improved patient outcomes.”
Understanding Liver Enzyme Tests and Markers
Liver enzyme tests are key in diagnosing and tracking autoimmune hepatitis. These blood tests give insights into the liver’s health and function. They help doctors see how severe the condition is and how it’s changing.
Interpreting Blood Test Results
People with autoimmune hepatitis often have high levels of liver enzymes like ALT and AST. These signs show liver damage and inflammation. Doctors watch these levels to see if treatments are working and to catch any problems early.
Significance of Autoantibodies
Autoantibodies are also crucial in diagnosing autoimmune hepatitis. These antibodies attack specific parts of liver cells. Knowing which autoantibodies are present helps doctors choose the right treatment.
Regular blood tests for liver enzymes and autoantibodies are vital for managing autoimmune hepatitis. Understanding these test results helps patients and doctors create effective treatment plans. This ensures the best care for those affected.
The Role of Liver Biopsy in Diagnosis
A liver biopsy is key in diagnosing liver inflammation and autoimmune hepatitis. It’s a small procedure that takes a piece of liver tissue. This tissue is then checked to find out why the liver isn’t working right.
Doctors usually suggest a liver biopsy when blood tests and other tests don’t give clear answers. By looking at the liver tissue, doctors can see signs of inflammation or scarring. These are common in autoimmune hepatitis.
The biopsy itself is usually safe, with only a small chance of problems like bleeding or infection. Before the biopsy, patients might have imaging tests. These tests help place the needle correctly and reduce risks.
The biopsy results help doctors understand how serious the liver disease is. They also guide treatment plans. People with autoimmune hepatitis might need to take medicines for a long time. The biopsy helps doctors choose the best treatment.
“A liver biopsy is a critical tool in the diagnosis and management of autoimmune hepatitis. It allows us to confirm the diagnosis and assess the extent of liver damage, which is essential for guiding treatment decisions.”
In short, a liver biopsy is very important for diagnosing liver inflammation and autoimmune hepatitis. It lets doctors see the liver up close. This helps them create a treatment plan that’s just right for each patient.
| Procedure | Description | Potential Risks |
|---|---|---|
| Liver Biopsy | A small sample of liver tissue is obtained using a hollow needle, typically guided by imaging techniques such as ultrasound or CT scan. | Bleeding, infection, pain, and in rare cases, organ puncture or internal bleeding. |
Treatment Options and Management Strategies
Treating autoimmune hepatitis needs a mix of treatments. This often includes immunosuppressants and corticosteroids. These medicines help control the immune system and reduce liver inflammation.
Initial Treatment Approaches
The main goal at first is to stop the disease from getting worse. Corticosteroids like prednisone are often used first. They are strong anti-inflammatory drugs that help calm down the immune system.
Long-term Management Plans
Once the initial treatment starts working, the focus turns to long-term care. Immunosuppressants like azathioprine are added to keep the disease in check. These medicines help keep the immune system from attacking the liver too much.
Monitoring Treatment Response
It’s important to keep an eye on how well the treatment is working. Liver tests and biopsies help check if the treatment is effective. They also help catch any problems early.
Managing autoimmune hepatitis is a team effort. With the right medicines and regular checks, patients can stay in remission. This improves their chances of a better future.
Medications and Immunosuppressive Therapy
Autoimmune hepatitis is treated with a mix of immunosuppressants and corticosteroids. These drugs calm down the immune system. They reduce inflammation and stop liver damage.
The main immunosuppressants for this condition are:
- Azathioprine
- 6-mercaptopurine
- Mycophenolate mofetil
These drugs slow down the immune system’s attack. They help keep liver enzymes stable. They work best with corticosteroids like prednisone. These steroids quickly ease symptoms and help the liver recover.
It’s key for patients to stick to their treatment plan. They should also go to regular check-ups. This way, doctors can adjust the doses as needed to keep the liver healthy.

“Careful monitoring and adjustment of medication dosages are essential to ensure the best possible outcomes for patients with autoimmune hepatitis.”
Knowing how immunosuppressants and corticosteroids help treat autoimmune hepatitis is important. It helps patients work with their doctors to find the best treatment for them.
Lifestyle Changes and Dietary Recommendations
Living with chronic hepatitis or liver disease means making healthy choices. Eating right and staying active helps your liver and overall health. Let’s look at important lifestyle changes and food tips that help.
Nutritional Guidelines
Eating a balanced diet is key for managing liver issues. Include these foods in your meals:
- Lean proteins like poultry, fish, and legumes help repair tissues and keep muscles strong
- Whole grains, fruits, and veggies are high in fiber, aiding digestion and blood sugar control
- Healthy fats from avocados, nuts, and olive oil fight inflammation and boost heart health
- Drink lots of water to flush out toxins and support liver health
Exercise and Activity Levels
Exercise is vital for liver health and well-being. Mix up your routine with aerobic, strength, and flexibility exercises:
- Do moderate aerobic activities like brisk walking, swimming, or cycling for 150 minutes weekly
- Include strength training with resistance bands or light weights to keep muscles and support liver
- Try gentle stretching and yoga to boost flexibility and lower stress
Always talk to your doctor before starting or changing your exercise plan. They can tailor advice based on your health and any medications.
Adopting these lifestyle and dietary changes can help those with chronic hepatitis or liver disease manage their condition better. It can also improve their quality of life.
Preventing Flare-ups and Managing Complications
Living with autoimmune hepatitis means staying alert and taking action. It’s key to stop flare-ups and handle complications to keep your liver healthy. This improves your life quality a lot.
Regular Monitoring and Checkups
Seeing your doctor often is vital. It helps track autoimmune hepatitis and catches liver inflammation early. You might need blood tests, scans, and liver biopsies to check your liver’s health.
Stress Management Techniques
Stress can make autoimmune hepatitis worse. Using stress-reducing methods like meditation, yoga, or deep breathing can help. These activities can improve your health and happiness.
Avoiding Alcohol and Certain Medications
Drinking alcohol and some medicines can hurt your liver more if you have autoimmune hepatitis. It’s important to stay away from alcohol and talk to your doctor before trying new medicines. This includes over-the-counter drugs and supplements.
By using these tips, people with autoimmune hepatitis can prevent flare-ups and manage complications. This helps them live a better life.
“Proactive management is the key to living well with autoimmune hepatitis.”
Living with Chronic Hepatitis: Long-term Outlook
Living with chronic hepatitis, including autoimmune hepatitis, can be challenging. But, with the right care and support, people can live full lives. The future looks different for everyone, based on how severe the condition is, how well treatment works, and overall health.
Quality of Life Considerations
Those with chronic hepatitis might feel tired, have stomach pain, or see yellow in their eyes. These symptoms can make everyday tasks hard. Yet, with the right treatment and lifestyle changes, many manage their symptoms well. It’s important to stick to treatment plans, eat right, and stay active to keep a good quality of life.
Support Systems and Resources
- Being part of a support group, online or in-person, can offer a sense of belonging. It helps with the emotional side of living with chronic hepatitis.
- Talking to doctors, like hepatologists and gastroenterologists, is key. They help understand the condition and find the right resources.
- Learning from trusted medical sources and patient groups can empower people. It helps them make informed choices about their health.
| Resource | Description | Contact Information |
|---|---|---|
| American Liver Foundation | National non-profit that offers education, support, and resources for liver diseases, including chronic hepatitis. | Phone: 1-800-465-4837 Website: www.liverfoundation.org |
| Autoimmune Hepatitis Association | Patient group that provides educational materials, support, and a network for autoimmune hepatitis. | Phone: 1-877-902-0859 Website: www.autoimmune-hepatitis.org |
By using support systems and resources, people with chronic hepatitis can manage their condition better. This helps them stay positive about their future health and well-being.
Conclusion
Autoimmune hepatitis is a complex liver condition that needs careful management and ongoing care. Early diagnosis and proper treatment are key to preventing liver damage. This ensures a good quality of life for those affected.
Understanding symptoms, causes, and treatment options is important. This way, individuals can work with their healthcare providers to create a management plan that fits their needs.
Maintaining regular check-ups and following prescribed medications are crucial. Making lifestyle adjustments also helps in managing autoimmune hepatitis. This can reduce the risk of complications.
Patients should seek medical advice if they think they might have this condition. Quick action can greatly improve their long-term outlook.
With the right care and support, people with autoimmune hepatitis can live fulfilling lives. They can manage their condition and keep their liver healthy. Staying informed and addressing challenges proactively helps patients achieve a better quality of life and a positive outlook for the future.
FAQ
Q: What is autoimmune hepatitis?
A: Autoimmune hepatitis is a chronic liver condition. It happens when the immune system attacks and damages liver cells. This leads to inflammation and impaired liver function.
Q: What are the symptoms of autoimmune hepatitis?
A: Symptoms include fatigue, jaundice (yellowing of the skin and eyes), and abdominal pain. Joint pain and nausea are also common.
Q: What causes autoimmune hepatitis?
A: The exact cause is not known. But it’s thought to involve genetics and environmental factors. These factors trigger the immune system to attack the liver.
Q: How is autoimmune hepatitis diagnosed?
A: Diagnosis involves blood tests, imaging studies, and a liver biopsy. Blood tests look for specific autoantibodies. A liver biopsy confirms the disease’s features.
Q: How is autoimmune hepatitis treated?
A: Treatment focuses on immunosuppressant medications, like corticosteroids. These drugs reduce inflammation in the liver. Long-term management may include other drugs and monitoring liver function.
Q: What is the long-term outlook for individuals with autoimmune hepatitis?
A: With proper treatment, many people can manage the condition well. They can live a good life. But, the condition is chronic. Regular monitoring and treatment adjustments are needed to prevent flare-ups and complications.
