Cardiac failure, or heart failure, is a major health issue worldwide. This condition greatly impacts people’s lives and costs the healthcare system about $30 billion each year.
This article aims to explain cardiac failure in detail. We’ll cover its definition, causes, symptoms, and the newest treatments. By understanding this heart condition better, readers can make smarter health choices.
Key Takeaways
- Cardiac failure is a serious and widespread heart condition that affects millions globally.
- Understanding the causes, symptoms, and impact of cardiac failure is crucial for effective management and treatment.
- Early diagnosis and a comprehensive approach to care, including lifestyle modifications and medical interventions, can significantly improve patient outcomes.
- Advancements in research and technology are continuously shaping the landscape of cardiac failure treatment, offering new hope for those living with this condition.
- Empowering individuals with knowledge about cardiac failure can help them make informed decisions and take an active role in their health and well-being.
What is Cardiac Failure: Definition and Overview
Cardiac failure, also known as heart failure, is a serious condition. The heart has trouble pumping blood around the body. This can cause cardiomyopathy (heart muscle disease) and ventricular dysfunction (heart ventricle problems).
Types of Heart Failure
There are different types of heart failure. These include left-sided, right-sided, and biventricular failure. Each type needs its own treatment plan.
Common Signs and Symptoms
- Shortness of breath, especially during physical activity
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Irregular heartbeat or palpitations
- Persistent cough or wheezing
Impact on Quality of Life
Cardiac failure can greatly affect a person’s life. It causes physical, emotional, and social problems. Patients may find it hard to move around, do daily tasks, and feel well overall. It’s important to manage heart muscle disease to improve their life quality.
| Symptom | Impact on Quality of Life |
|---|---|
| Shortness of breath | Limits physical activity and daily tasks |
| Fatigue and weakness | Reduces energy levels and overall functionality |
| Swelling in limbs | Discomfort and difficulty with mobility |
“Cardiac failure is a complex condition that requires a holistic approach to management, addressing both the physical and emotional well-being of the patient.”
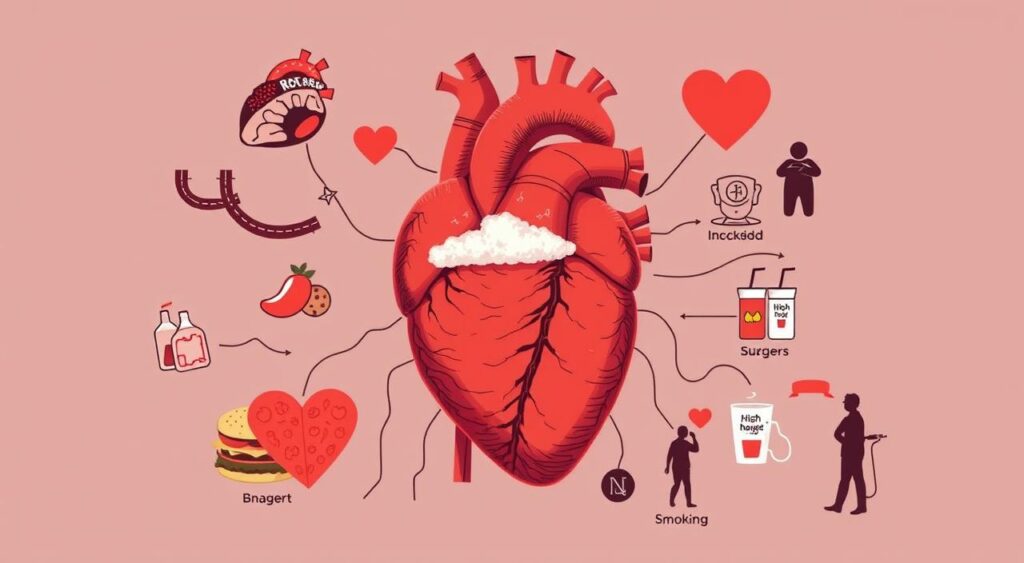
Risk Factors Contributing to Heart Failure
It’s important to know what increases the risk of heart failure. Some risks, like age and family history, can’t be changed. But, there are things we can control to lower our risk of heart problems, including diastolic dysfunction and systolic dysfunction.
Hypertension, or high blood pressure, is a big risk factor. It can make the heart muscle weak and stiff. This makes it hard for the heart to pump blood well. Diabetes is also a big risk because high blood sugar can harm the heart and blood vessels.
Being overweight, not being active, and eating poorly can also lead to heart failure. These habits can raise the risk of other health issues like high cholesterol and heart disease. These problems can damage the heart and lead to dysfunction.
Some medical conditions, like heart valve problems and heart muscle diseases, also increase the risk of heart failure. Knowing these risks and making lifestyle changes can help prevent or slow down heart failure.
“The key to managing heart failure is to identify and address the underlying risk factors before the condition becomes severe.”
Learning about heart failure risks can help us protect our hearts. By making healthy choices and staying informed, we can lower our risk of heart failure.
Common Causes of Cardiac Failure
Cardiac failure is when the heart can’t pump blood well. It comes from many medical issues and lifestyle choices. Knowing what causes it is key to fighting this big health problem.
Medical Conditions Leading to Heart Failure
Coronary artery disease is a big cause. It happens when heart arteries get narrow or blocked. This makes the heart pump less well. Hypertension, or high blood pressure, also strains the heart. It can weaken the heart muscle and lead to failure.
Valvular heart diseases, like mitral or aortic valve problems, also play a part. They make it hard for the heart to move blood around.
Lifestyle Factors and Their Impact
Some lifestyle choices can hurt your heart. Smoking and too much alcohol can damage the heart muscle. A life sitting down and eating too much salt or fat can also harm your heart.
These habits can lead to obesity and diabetes. Both can increase the risk of heart failure.
Genetic Predisposition
Genetics can also play a role. Some cardiomyopathies, or heart muscle diseases, are passed down. They can make the heart weak or big, making it hard to pump blood.
Knowing your family’s heart health history is important. It helps doctors and patients watch for and manage heart failure risks.
| Cause | Description | Impact on Ejection Fraction |
|---|---|---|
| Coronary Artery Disease | Narrowing or blockage of the arteries supplying blood to the heart | Reduced ejection fraction, leading to decreased cardiac output |
| Hypertension | High blood pressure that stresses the heart muscle | Decreased ejection fraction due to left ventricular hypertrophy |
| Valvular Heart Diseases | Conditions affecting the heart’s valves, such as mitral or aortic valve disorders | Impaired cardiac output and reduced ejection fraction |
| Genetic Cardiomyopathies | Inherited diseases of the heart muscle, leading to weakened or enlarged heart | Decreased ejection fraction and impaired cardiac function |
Understanding the many causes of cardiac failure helps doctors find better ways to treat it. This is especially true for end-stage heart failure.
Diagnosis Methods and Testing
Getting a correct diagnosis is key to treating cardiac failure. Doctors use many methods to check the heart and plan treatment. These include physical exams, lab tests, and imaging.
A doctor starts with a physical exam. They listen to the heart, check for fluid, and look for signs of trouble. Blood tests also help, showing biomarkers that show cardiac failure or cardiomyopathy.
Imaging is very important for diagnosing heart failure. Echocardiograms use sound waves to see the heart’s shape and how it works. Magnetic Resonance Imaging (MRI) gives detailed pictures, showing how bad cardiac failure is and what might be causing it.
In some cases, a cardiac catheterization is needed. This is when a thin tube is put into a blood vessel to check the heart’s pressure and function. It helps doctors know exactly what’s wrong and how to fix it.
It’s very important to diagnose cardiac failure early and correctly. Doctors use many tools to understand the heart’s condition. This helps them create a treatment plan that works best for each patient.
| Diagnostic Method | Description | Insights Provided |
|---|---|---|
| Physical Examination | A thorough physical assessment, including listening to heart sounds and checking for fluid buildup | Initial signs and symptoms of cardiac failure |
| Blood Tests | Measuring levels of biomarkers that indicate the presence and severity of heart failure | Severity and underlying causes of cardiac failure |
| Echocardiogram | Using sound waves to create images of the heart, evaluating its structure and function | Abnormalities in the heart’s structure and performance |
| Cardiac MRI | Providing detailed, high-resolution images of the heart and its surrounding tissues | Extent and causes of cardiac failure |
| Cardiac Catheterization | Inserting a thin, flexible tube into a blood vessel to measure the heart’s pressure and function directly | Precise measurements of the heart’s performance and suitability for specific treatments |
By using different tests, doctors can fully understand cardiac failure or cardiomyopathy. This helps them make the best treatment plan. It also improves the patient’s life quality.
Understanding Different Stages of Heart Failure
Congestive heart failure gets worse over time. Knowing the stages is key to managing it well. The New York Heart Association (NYHA) and the American College of Cardiology/American Heart Association (ACC/AHA) systems help classify congestive heart failure, ventricular dysfunction, and ejection fraction.
Early Stage Symptoms
In the early stages, symptoms are mild. You might feel short of breath when active, tired, or have swelling in your legs. These can be managed with lifestyle changes and medicine, and your heart’s ejection fraction might still be normal.
Progressive Stage Indicators
- As heart failure gets worse, symptoms get more severe. You might always feel short of breath, tired, and have more swelling in your legs and feet.
- The heart’s ventricular dysfunction gets worse, lowering your ejection fraction.
- You might find it hard to do daily tasks and need to avoid too much physical activity.
Advanced Stage Management
In the advanced stages, symptoms are severe. You might always feel short of breath, extremely tired, and have a lot of fluid buildup. You’ll need a full treatment plan, including medicines, devices, and sometimes surgery, to manage it and improve your life.
| Stage | Symptoms | Ejection Fraction | Treatment Approach |
|---|---|---|---|
| Early | Mild, manageable | Normal | Lifestyle changes, medication |
| Progressive | Worsening, limiting daily activities | Decreased | Medication, device therapies |
| Advanced | Severe, debilitating | Significantly decreased | Comprehensive medical treatment, including medications, devices, and sometimes surgery |
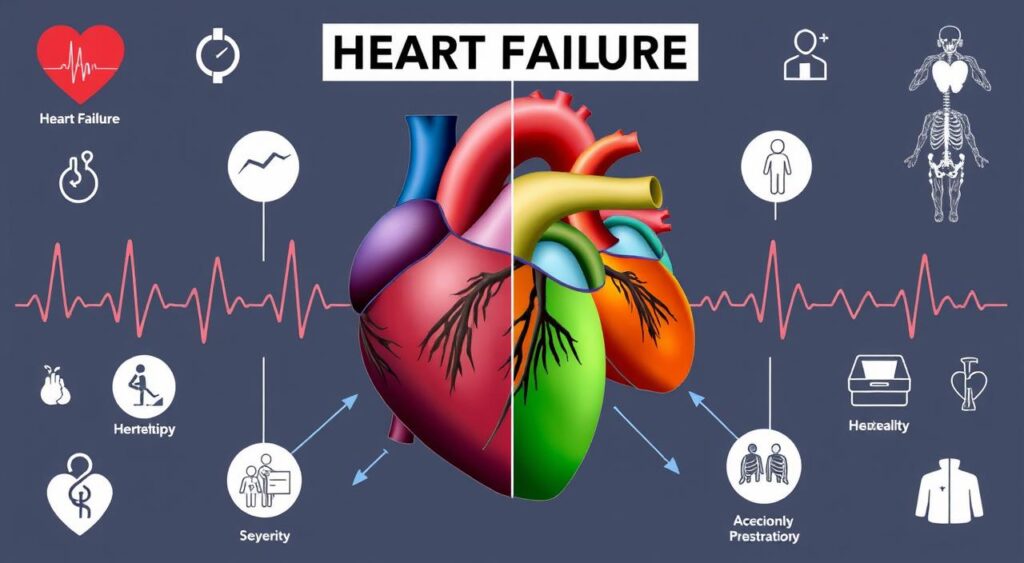
Understanding heart failure’s stages helps both you and your doctor plan the best care. This way, you can tackle the challenges of each stage effectively.
Treatment Options and Management Strategies
Managing cardiac failure needs a team effort. It can come from heart muscle disease, diastolic dysfunction, or systolic dysfunction. The goal is to ease symptoms, boost quality of life, and slow disease progress.
Medicine is key in treating cardiac failure. ACE inhibitors, ARBs, beta-blockers, and diuretics help the heart work better. They also reduce fluid and manage symptoms. The right mix of medicines depends on the patient and their heart failure stage.
Lifestyle changes are also vital. Eating right, exercising, and managing stress are important. These steps help control symptoms, stop the disease from getting worse, and improve health.
For serious cases, surgery might be needed. Coronary artery bypass grafting, valve repair or replacement, and devices like pacemakers or ICDs can help. These surgeries aim to improve heart function and lower risks.
Managing cardiac failure well needs a team. Cardiologists, primary care doctors, nurses, and others work together. This team approach ensures the best care for each patient.
Medication Management Strategies
- ACE inhibitors and ARBs to improve heart function and reduce fluid buildup
- Beta-blockers to slow heart rate and decrease the workload on the heart
- Diuretics to help eliminate excess fluid and alleviate symptoms
- Individualized medication regimens tailored to the patient’s specific needs
Lifestyle Modifications
- Adopt a heart-healthy diet rich in fruits, vegetables, and whole grains
- Engage in regular physical activity within the patient’s capabilities
- Manage stress levels through relaxation techniques and mental health support
Surgical Interventions
| Procedure | Purpose |
|---|---|
| Coronary Artery Bypass Grafting | Improve blood flow to the heart |
| Valve Repair or Replacement | Restore normal heart valve function |
| Pacemaker or ICD Implantation | Regulate heart rhythm and prevent complications |
A complete treatment plan is key. It tackles the heart failure’s root causes. This way, healthcare providers can help patients feel better, manage symptoms, and live better lives.
“Effective management of cardiac failure requires a collaborative effort between healthcare professionals, focusing on both medical interventions and lifestyle modifications to address the unique needs of each patient.”
Lifestyle Changes and Prevention Methods
Keeping a healthy lifestyle is key for those with cardiac failure or at risk. Simple changes can greatly improve life quality and slow heart failure’s progress.
Dietary Recommendations
Eating right is vital for heart health. Experts suggest a diet full of:
- Fruits and vegetables
- Whole grains
- Lean proteins (e.g., fish, poultry, legumes)
- Healthy fats (e.g., avocados, nuts, olive oil)
It’s also important to cut down on sodium, saturated fats, and sugars. These can make heart failure worse.
Exercise Guidelines
Regular exercise strengthens the heart and boosts health. Those with cardiac failure should work with doctors to create a safe plan. This might include:
- Moderate-intensity aerobic exercises, such as walking, swimming, or cycling
- Strength training exercises to build muscle and improve overall fitness
- Flexibility and balance exercises to maintain mobility and prevent falls
Start slow and gradually increase workout intensity as you get stronger.
Stress Management Techniques
Stress can harm the heart and worsen cardiac failure. Using stress management techniques daily can help:
- Mindfulness meditation
- Deep breathing exercises
- Yoga or tai chi
- Engaging in hobbies and leisure activities
- Seeking support from friends, family, or support groups
By adopting these lifestyle changes, individuals can manage their health better and improve their well-being.
| Lifestyle Factor | Recommendation | Potential Impact |
|---|---|---|
| Diet | Whole, unprocessed foods; limit sodium, saturated fats, and added sugars | Improved heart health, reduced symptom severity |
| Exercise | Moderate-intensity aerobic, strength training, and flexibility exercises | Strengthened heart muscle, improved cardiovascular fitness |
| Stress Management | Mindfulness, deep breathing, yoga, hobbies, and social support | Reduced stress levels, improved emotional well-being |
“Making lifestyle changes can be challenging, but they are essential for managing cardiac failure and improving overall health. With the right support and guidance from healthcare providers, patients can take control of their condition and work towards a better quality of life.”
Living with Cardiac Failure: Long-term Outlook
Life with cardiac failure, like congestive heart failure or cardiomyopathy, is tough. But, with the right care and lifestyle changes, many people can live well and manage their heart condition.
The future looks different for each person with cardiac failure. It depends on the cause, how severe it is, and how well treatment works. The heart’s pumping ability, measured by ejection fraction, is key in planning treatment and predicting outcomes.
Keeping an eye on your heart health and working closely with a cardiologist is crucial. You might need tests like echocardiograms or stress tests to check how your heart is doing. This helps your doctor adjust your treatment plan as needed.
Support and Coping Strategies
Heart conditions can be hard on the mind and heart. Getting help from doctors, joining support groups, and finding ways to reduce stress are very helpful.
- Talking to others who know what you’re going through can make you feel less alone.
- Doing things that calm your mind, like meditation or yoga, can help with the emotional side of heart failure.
- Learning more about your condition and treatment options can help you feel more in control of your care.
With the right support and a positive attitude, many people can live full lives despite heart failure. Staying informed, following your treatment plan, and taking care of yourself are key. This way, you can face the future with hope and positivity.
| Condition | Description | Prognosis |
|---|---|---|
| Congestive Heart Failure | A chronic condition where the heart’s ability to pump blood effectively is impaired, leading to fluid buildup and various symptoms. | With proper management, many patients with congestive heart failure can maintain a good quality of life, though the long-term outlook depends on the underlying cause and severity of the condition. |
| Cardiomyopathy | A disease that affects the heart muscle, making it harder for the heart to pump blood efficiently. This can lead to cardiac failure. | The prognosis for individuals with cardiomyopathy varies depending on the type and severity of the condition. Early diagnosis and appropriate treatment can help manage symptoms and slow the progression of the disease. |
“With the right support and a proactive approach, patients can navigate the long-term journey with cardiac failure and lead fulfilling lives.”
Understanding your condition and actively managing it can greatly improve your life. It helps you stay positive and hopeful, even with a chronic condition.
Conclusion
Cardiac failure, or heart failure, is a complex condition. It needs a deep understanding of its causes, symptoms, and treatments. This journey has shown how crucial early detection and proper management are for those with heart muscle disease.
Knowing the risk factors and causes of cardiac failure is key. This includes medical conditions, lifestyle choices, and genetics. By addressing these, people can prevent or delay heart failure.
Healthcare professionals use various tests to diagnose heart failure. These tests help them create personalized treatment plans. This is crucial for managing the condition effectively.
Living with cardiac failure is tough, but there’s hope. Medical research and new treatments offer better outcomes and quality of life. By focusing on heart health, people with cardiac failure can face the future with optimism.
FAQ
Q: What is cardiac failure?
A: Cardiac failure, also known as heart failure, is when the heart can’t pump blood well. This leads to symptoms and health issues that affect a person’s life quality.
Q: What are the different types of heart failure?
A: Heart failure types include left-sided, right-sided, and biventricular failure. Left-sided failure means the left ventricle can’t pump blood to the body. Right-sided failure affects the right ventricle’s ability to pump blood to the lungs. Biventricular failure means both ventricles don’t work right.
Q: What are the common signs and symptoms of cardiac failure?
A: Signs of heart failure include shortness of breath and fatigue. Swelling in the legs and feet, irregular heartbeat, and trouble sleeping are also common. It can make it hard to do physical activities and lower quality of life.
Q: What are the risk factors for developing heart failure?
A: Risk factors for heart failure include age and family history. Hypertension, diabetes, obesity, smoking, and poor diet are also risks. Knowing these can help prevent and treat the condition early.
Q: What are the leading causes of cardiac failure?
A: Heart failure is often caused by coronary artery disease, hypertension, and valvular heart disease. Lifestyle choices like smoking and poor diet can also contribute. Genetics can play a role in some cases.
Q: How is cardiac failure diagnosed?
A: Doctors use physical exams, blood tests, and imaging like echocardiograms and MRIs to diagnose heart failure. Cardiac catheterization is also used. Early and accurate diagnosis is key for treatment.
Q: What are the different stages of heart failure?
A: Heart failure stages range from early symptoms to advanced management. The New York Heart Association (NYHA) and American College of Cardiology/American Heart Association (ACC/AHA) systems help classify the stages.
Q: What are the treatment options for cardiac failure?
A: Treatments include medications, lifestyle changes, and surgery. A team of doctors and specialists work together for the best care.
Q: What lifestyle changes can help manage cardiac failure?
A: Eating a heart-healthy diet and exercising regularly can help. Stress management is also important. Patient education and self-care are key to managing the condition.
Q: What is the long-term outlook for patients with cardiac failure?
A: The outlook depends on the condition’s severity, cause, and treatment. While heart failure is chronic, proper management and lifestyle changes can improve quality of life and outcomes.
