Did you know cirrhosis of the liver is a major cause of death worldwide ? It claims over 1 million lives each year. This chronic liver disease often goes unnoticed until it’s too late. Knowing the causes and treatments for cirrhosis is key to fighting this condition and improving liver health.
Cirrhosis is a serious condition where the liver gets scarred and damaged. This makes it hard for the liver to work right. It can cause serious problems like portal hypertension and liver failure if not treated. In this article, we’ll explore the causes, symptoms, diagnosis, and treatment options for cirrhosis. This will help you take steps to protect your liver health.
Key Takeaways
- Cirrhosis is a leading cause of death worldwide, affecting over 1 million people annually.
- The liver becomes scarred and damaged, impairing its ability to function properly.
- Understanding the causes and available treatments is crucial for managing this chronic liver disease.
- Early detection and intervention can significantly improve liver health outcomes.
- Lifestyle changes and adherence to treatment plans are essential for managing cirrhosis.
What is Cirrhosis of Liver: Definition and Overview
Cirrhosis of the liver is a serious condition where the liver gets scarred and damaged. This damage is permanent and happens over time. The liver tries to fix itself but ends up getting worse.
The scarring, or liver fibrosis, makes the liver lose its function. If not treated, it can turn into end-stage liver disease.
Understanding the Liver Scarring Process
When the liver gets hurt a lot, like from drinking too much alcohol or viruses, it tries to heal. This healing makes scar tissue, or fibrosis, which takes the place of healthy liver cells. Over time, this scarring builds up and messes with the liver’s normal work.
Stages of Liver Disease Progression
Liver disease goes through stages, starting with inflammation, then fibrosis, and finally cirrhosis. As it gets worse, the liver gets more scarred and nodular. This makes it hard for the liver to do its important jobs.
Impact on Liver Function
Cirrhosis makes the liver lose its ability to do its vital tasks. It can’t break down drugs and toxins, make important proteins, or help with blood clotting. This decline in liver function can cause serious problems and, if not treated, can be deadly.
| Key Characteristic | Description |
|---|---|
| Liver Scarring | Cirrhosis is characterized by the progressive replacement of healthy liver tissue with scar tissue, known as fibrosis. |
| Impaired Liver Function | As the liver becomes more scarred, its ability to perform essential functions, such as metabolizing drugs and producing crucial proteins, is compromised. |
| Liver Failure | If left untreated, cirrhosis can lead to the complete failure of the liver, a life-threatening condition known as end-stage liver disease. |
Common Causes and Risk Factors
Cirrhosis of the liver is a serious disease that causes scarring and damage. It has many causes. Knowing these causes and risk factors is key to preventing and managing the disease.
Chronic alcohol abuse is a major cause of cirrhosis. Drinking too much alcohol over time harms liver cells. Viral hepatitis, especially Hepatitis B and C, also leads to cirrhosis.
Non-alcoholic fatty liver disease (NAFLD) is another common cause. It happens when fat builds up in the liver, leading to inflammation and scarring. NAFLD is linked to obesity, type 2 diabetes, and metabolic syndrome.
Other causes of cirrhosis include:
- Autoimmune disorders, such as primary biliary cholangitis and primary sclerosing cholangitis
- Genetic disorders, like hemochromatosis and Wilson’s disease
- Bile duct blockages or damage
- Exposure to certain toxins or medications
Some risk factors increase the chance of getting liver disease and cirrhosis. These include:
- Age (cirrhosis is more common in older adults)
- Obesity and metabolic syndrome
- Diabetes
- Certain ethnic or genetic backgrounds
- Exposure to environmental toxins or pollutants
Healthcare professionals can better help people at risk by knowing the causes and risk factors of cirrhosis. They can then take steps to prevent and treat the disease early.
| Cause | Prevalence | Risk Factors |
|---|---|---|
| Alcohol Abuse | 40-50% | Excessive, long-term alcohol consumption |
| Viral Hepatitis | 20-30% | Chronic Hepatitis B or C infection |
| Non-Alcoholic Fatty Liver Disease (NAFLD) | 10-20% | Obesity, diabetes, metabolic syndrome |
| Other Causes | 10-20% | Autoimmune disorders, genetic conditions, bile duct issues, toxin exposure |
By understanding the causes and risk factors of chronic liver damage and liver disease, healthcare professionals can create better prevention and treatment plans. This is crucial for tackling this major public health issue.
Signs and Symptoms of Liver Cirrhosis
It’s important to know the early signs and symptoms of cirrhosis of the liver. This liver disease can start quietly, but noticing these signs early is key. It helps in getting medical help quickly.
Early Warning Signs
- Fatigue and weakness
- Loss of appetite or feeling full quickly
- Nausea and vomiting
- Abdominal discomfort or pain
- Swelling in the legs or abdomen
Advanced Symptoms
As cirrhosis gets worse, symptoms can get more serious. People might notice:
- Jaundice: Yellowing of the skin and eyes due to the buildup of bilirubin
- Bleeding and bruising easily
- Confusion, memory lapses, and changes in personality (hepatic encephalopathy)
- Fluid accumulation in the abdomen (ascites)
- Gastrointestinal bleeding from enlarged veins in the esophagus or stomach
When to Seek Medical Attention
If you notice any of these signs or symptoms, get medical help right away. Early treatment can greatly improve life for those with cirrhosis of the liver. Always talk to a doctor for a full check-up and a treatment plan that fits you.
Diagnosis Methods and Tests
Diagnosing liver cirrhosis requires a detailed look at several tests. It’s important to get it right to treat the disease well.
Blood Tests
Blood tests are key in checking how well the liver works. They look for signs of cirrhosis. Tests include:
- Liver enzyme tests (ALT, AST, ALP, GGT)
- Bilirubin levels
- Prothrombin time (PT) and international normalized ratio (INR)
- Albumin levels
Imaging Studies
Imaging tests give a clear view of the liver’s health. They are:
- Ultrasound: Checks liver size, texture, and blood flow
- Computed Tomography (CT) scan: Shows detailed liver and surrounding images
- Magnetic Resonance Imaging (MRI): Gives high-quality images of liver fibrosis and cirrhosis
Liver Biopsy
A liver biopsy might be needed to confirm cirrhosis. It takes a small liver sample for a microscope check. This test shows how bad the liver fibrosis and cirrhosis of the liver are.
| Diagnostic Test | Purpose | Advantages | Limitations |
|---|---|---|---|
| Blood Tests | Assess liver function and detect signs of cirrhosis | Non-invasive, widely available, and cost-effective | May not provide a definitive diagnosis on their own |
| Imaging Studies | Evaluate liver structure, size, and blood flow | Can detect early signs of liver disease and cirrhosis | May not accurately measure the extent of liver fibrosis |
| Liver Biopsy | Confirm the diagnosis and assess the severity of cirrhosis | Provides a direct assessment of liver tissue | Invasive procedure with a small risk of complications |
By using these tests together, doctors can accurately find liver fibrosis and cirrhosis of the liver. This helps start the right treatment quickly.
“Early detection and accurate diagnosis are crucial in managing liver cirrhosis effectively and preventing further complications.”
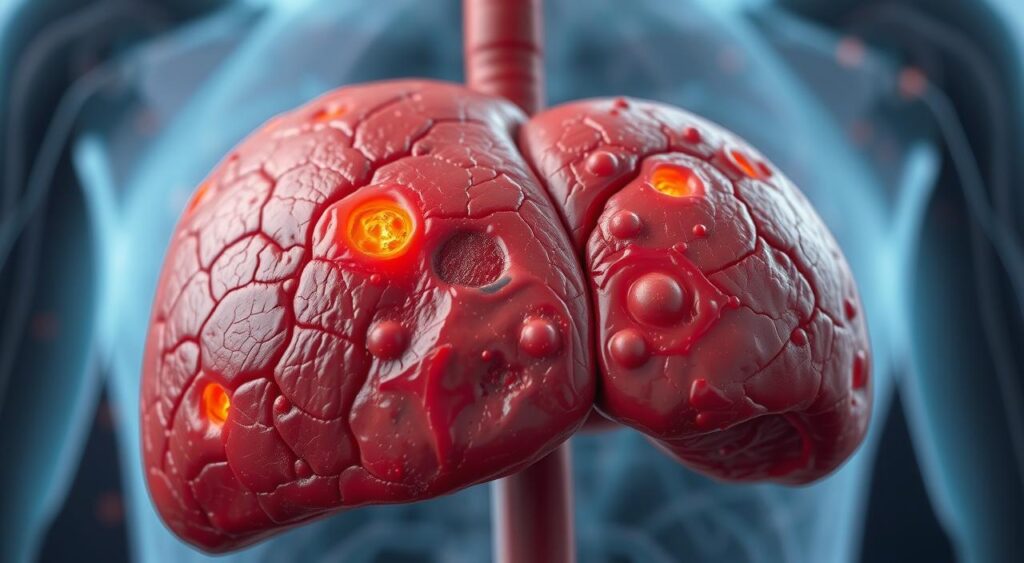
Complications of Advanced Liver Disease
As cirrhosis of the liver gets worse, serious complications can happen. These problems come from too much pressure in the liver, blocking blood flow. It’s key to know about these issues to manage liver disease well.
Portal Hypertension
Portal hypertension is a big problem in advanced cirrhosis. It happens when liver scarring blocks blood flow in the portal vein. This vein carries blood from the digestive system to the liver. The high pressure can cause new blood vessels to form in the esophagus, stomach, and rectum.
Esophageal Varices
Esophageal varices are a serious issue from too much pressure. These are big, twisted veins in the esophagus. They can burst, causing severe bleeding. It’s very important to catch and treat esophageal varices early.
Hepatic Encephalopathy
Liver cirrhosis can also mess up the liver’s job of removing toxins. This leads to hepatic encephalopathy. It causes confusion, disorientation, and can even lead to coma. It’s vital to treat hepatic encephalopathy quickly to stop brain damage.
Dealing with these complications is a big part of managing cirrhosis. Patients and doctors need to work together. They must watch for these problems and take steps to reduce risks and improve health.
Treatment Options and Management Strategies
For those with cirrhosis of the liver, a detailed treatment plan is key. It helps manage the condition and stops further damage. While a liver transplant is the best option for severe cases, other treatments can slow disease progress and enhance life quality.
Medication Management
Patients with cirrhosis may take various medicines. These include diuretics for fluid buildup, antibiotics for infections, and laxatives for constipation. Some drugs also help lower pressure in the liver to prevent bleeding.
Lifestyle Modifications
Changing your lifestyle can also help manage cirrhosis. Eating a balanced diet, avoiding alcohol, and staying active support liver health. These actions can slow disease progress.
Liver Transplantation
For those with severe liver disease, a liver transplant might be the best choice. This surgery replaces the damaged liver with a healthy one. It can greatly improve life expectancy and quality of life.
| Treatment Option | Description | Potential Benefits |
|---|---|---|
| Medication Management | Prescription of various medications to address complications and support liver function | Helps manage symptoms, prevent infections, and reduce the risk of complications |
| Lifestyle Modifications | Adoption of a healthy diet, limited alcohol consumption, and appropriate physical activity | Can help slow disease progression and improve overall health |
| Liver Transplantation | Replacement of the damaged liver with a healthy one, either from a living or deceased donor | Significantly improves survival rates and quality of life for those with end-stage liver disease |
Combining medical treatments, lifestyle changes, and sometimes liver transplantation can manage cirrhosis. Regular check-ups and teamwork between patients and healthcare providers are vital. This approach helps manage the condition effectively.
“Liver transplantation can be a life-saving procedure for individuals with end-stage liver disease, providing them with a second chance at a healthy life.”
Lifestyle Changes and Dietary Recommendations
Managing liver disease and cirrhosis needs a big change in lifestyle. This includes following nutritional guidelines, exercising right, and avoiding alcohol and harmful substances. These steps are key to managing the condition well.
Nutrition Guidelines
Eating a balanced diet is crucial for those with liver disease or cirrhosis. Here are some dietary tips:
- Eat lots of whole, unprocessed foods like fruits, veggies, whole grains, and lean proteins.
- Watch your sodium intake to prevent fluid buildup and swelling.
- Boost your protein to help your liver work better and repair tissues.
- Avoid foods high in fat, sugar, and fried items that can harm your liver.
- Drink plenty of water to stay hydrated.
Exercise and Activity Limitations
Exercise is good for liver disease or cirrhosis, but do it carefully. Follow your doctor’s advice. Here’s what to keep in mind:
- Start with low-impact activities like walking, swimming, or gentle yoga to avoid too much strain.
- Slowly increase how long and hard you exercise, as your body allows.
- Stay away from activities that could hurt you or strain your liver more, like contact sports or very hard workouts.
- Talk to your doctor often to make sure your exercise plan is safe and right for you.
Alcohol and Substance Avoidance
For those with liver disease or cirrhosis, staying away from alcohol and harmful substances is very important. Alcohol can hurt your liver more, and some medicines or substances can interact badly with a sick liver. It’s vital to:
- Not drink alcohol at all.
- Tell your doctor about all medicines, supplements, and substances you use to manage them safely.
- Look for help and resources if you need to stop drinking or using substances.
By making these lifestyle changes and following these dietary tips, people with liver disease or cirrhosis can help manage their condition. They can support their health and maybe slow down the disease’s progress.
Prevention Strategies and Risk Reduction
Liver fibrosis and chronic liver damage can be prevented or slowed. Healthy lifestyle choices and addressing risk factors help. This way, people can lower their chance of getting cirrhosis of the liver.
Vaccination and Viral Infection Prevention
Protecting against viral hepatitis infections is key to preventing liver fibrosis. Vaccination for hepatitis A and B gives lifelong protection. Safe sex and avoiding needle-sharing also prevent hepatitis C, a major cause of cirrhosis.
Alcohol Moderation and Abstinence
Too much alcohol harms the liver and can lead to cirrhosis. Drinking less or not drinking at all helps a lot. Getting help for alcohol addiction is also important for liver health.
Healthy Lifestyle Choices
- Eating a balanced diet with fruits, veggies, and whole grains is good for the liver.
- Regular exercise helps manage conditions like obesity and diabetes, which harm the liver.
- Staying away from illicit drugs and certain meds that stress the liver is also wise.
Preventing viral infections, drinking in moderation, and living healthily reduce cirrhosis risk. These steps help keep the liver healthy.

“Prevention is better than cure when it comes to liver disease. By making informed choices and addressing the root causes, we can safeguard our liver health and avoid the complications of cirrhosis.”
Living with Liver Cirrhosis: Daily Management Tips
Living with end-stage liver disease, or cirrhosis, can be tough. But, with the right strategies, you can manage your condition and live better. Here are some practical tips for daily life with liver cirrhosis.
Medication Management
It’s key to keep up with your medications if you have cirrhosis. Work with your healthcare team to make sure you’re taking the right meds at the right times. Use reminders, pill organizers, and keep a list of your meds to avoid mistakes.
Symptom Monitoring
Watch for any changes in your body and tell your doctor right away. Look out for fluid buildup, changes in thinking, and unusual bleeding or bruising. Tracking your symptoms helps your healthcare team make better decisions for you.
Stress Management
Dealing with a chronic condition like cirrhosis can be emotionally hard. Try stress-reducing activities like meditation, yoga, or gentle exercise. Also, consider joining a support group to connect with others who face similar challenges.
Dietary Adjustments
Eating a healthy, liver-friendly diet is crucial for those with cirrhosis. Work with a registered dietitian to create a meal plan that supports your health. This might mean eating less sodium, protein, and certain nutrients to help your liver.
By following these daily tips, you can actively manage your end-stage liver disease or cirrhosis. This can greatly improve your overall well-being.
Conclusion
Cirrhosis of the liver is a serious condition that needs careful management and lifestyle changes. Early detection and quick medical action are key to slowing liver scarring. This helps keep the liver working well.
Knowing the causes and signs of liver disease is important. Following proven treatment plans can improve life quality and lower the risk of serious problems. Eating right, exercising, and avoiding alcohol are crucial for managing cirrhosis.
Living with liver disease comes with challenges, but with the right support, people can manage their condition. Healthcare teams and self-care efforts can help slow liver disease. This empowers individuals to live better and face a brighter future with cirrhosis of the liver.
FAQ
Q: What is cirrhosis of the liver?
A: Cirrhosis is a long-term liver problem. It causes the liver tissue to scar and harden. This can make the liver not work right.
Q: What are the common causes of cirrhosis?
A: Cirrhosis often comes from drinking too much alcohol, hepatitis B or C, and non-alcoholic fatty liver disease (NAFLD). Other causes include autoimmune diseases, genetic issues, and bile duct problems.
Q: What are the symptoms of cirrhosis?
A: Early cirrhosis might not show symptoms. But as it gets worse, you might feel tired, lose your appetite, and get sick to your stomach. You could also swell in your legs or belly and turn yellow.
In the worst cases, you might get high blood pressure in your liver, bleeding in your esophagus, or brain problems.
Q: How is cirrhosis diagnosed?
A: Doctors use your medical history, a physical check-up, blood tests, and imaging like ultrasound or CT scans to find cirrhosis. They might also take a liver biopsy to see how damaged it is.
Q: What are the treatment options for cirrhosis?
A: Treatment depends on why you have cirrhosis and how bad it is. You might take medicine to feel better, change your lifestyle, or get a liver transplant if it’s very severe.
Q: Can cirrhosis be prevented?
A: Yes, you can lower your risk of cirrhosis. Don’t drink too much alcohol, get the hepatitis B vaccine, stay at a healthy weight, and manage any health problems that could harm your liver.
Q: How can someone with cirrhosis manage their condition daily?
A: Managing cirrhosis daily means taking your medicine, watching for symptoms, eating right, and making lifestyle changes. This includes eating less salt and protein, avoiding alcohol, and doing light exercise when you can.
