Comprehensive guide to Deep Tissue Injury: symptoms, treatment, and recovery strategies explained.
Pressure ulcers: These wounds, often caused by prolonged pressure on the skin, can lead to severe complications if not treated properly. Among them, deep tissue injury stands out as a critical concern in wound care.
Deep tissue injury refers to damage beneath the skin’s surface, often caused by sustained pressure or shear forces. Unlike superficial wounds, it may not be immediately visible, making early detection challenging. Non-blanchable skin discoloration and muscle damage are key early signs.
Historically, understanding and managing this condition has evolved significantly. Today, it remains a priority in healthcare due to its potential to develop into severe pressure injuries. This guide will explore symptoms, risk factors, and effective treatment strategies to help you stay informed.
Key Takeaways
- Deep tissue injury is a serious condition often caused by prolonged pressure.
- Early signs include non-blanchable skin discoloration and muscle damage.
- Pressure ulcers affect millions annually in the U.S.
- Proper wound care and early detection are crucial for prevention.
- Understanding risk factors can help reduce the likelihood of severe complications.
Understanding Deep Tissue Injury
Understanding the complexities of pressure-related wounds is essential for effective care. These conditions often develop due to prolonged exposure to pressure, leading to damage beneath the skin’s surface. Recognizing the signs early can prevent severe complications.
Definition and Clinical Overview
According to clinical guidelines, this condition involves damage to underlying tissue caused by sustained pressure or shear forces. Unlike superficial wounds, it may not be immediately visible, making early detection challenging. Non-blanchable discoloration and muscle damage are key indicators.
Patient history plays a crucial role in diagnosis. Factors like prolonged immobility, skin changes, and exposure to pressure events are critical. Clinicians often rely on a combination of visual assessment and patient-reported symptoms to identify the condition accurately.
Historical Context and Current Trends
Historically, the understanding of this condition has evolved significantly. Early methods focused on symptom management, while modern practices emphasize prevention and early intervention. Today, clinical guidelines recommend regular assessments for at-risk patients.
Current trends highlight the importance of tailored care plans. For example, patients with darker skin tones may present differently, requiring specialized diagnostic approaches. Advances in wound care technology have also improved outcomes for affected individuals.
Identifying Symptoms and Signs
Skin changes like purple or maroon hues often signal underlying issues. These visual cues are critical for identifying pressure-related wounds early. Recognizing these signs can prevent complications and improve outcomes.
Visual Indicators and Early Warning Signs
Early signs of pressure-related damage include purple or maroon discoloration. This often appears as a distinct area on the skin. Unlike superficial wounds, these changes may not blanch when pressed.
Defined borders around the affected area are another key indicator. Clinicians also look for subtle changes in skin texture. These signs help differentiate pressure-related wounds from other skin lesions.
Variations in Skin Discolouration and Presentation
Skin discoloration can vary based on factors like skin tone and wound progression. For example, darker skin tones may show purple or maroon hues more prominently. Superficial skin alterations, such as redness, may also be present.
It’s important to assess these changes carefully. They can help determine the stage pressure of the wound. This information guides treatment decisions and improves care outcomes.
| Wound Type | Characteristics | Key Differences |
|---|---|---|
| Pressure Ulcer | Purple/maroon discoloration, defined borders | Damage beneath the skin’s surface |
| Incontinence-Associated Dermatitis | Redness, irritation, no defined borders | Superficial skin damage |
| Skin Tears | Open wounds, irregular edges | Trauma-induced, not pressure-related |
Risk Factors and Patient Considerations
Identifying the factors that increase the risk of pressure-related wounds is crucial for effective prevention. Certain patient conditions and behaviors can significantly heighten the likelihood of developing serious skin issues. Understanding these risks helps in tailoring care plans and improving outcomes.
Key Patient Risk Factors
Several factors predispose individuals to pressure-related complications. Immobility is a primary concern, as it leads to prolonged exposure to pressure. Poor perfusion, often seen in patients with diabetes or vascular diseases, exacerbates the risk by reducing blood flow to soft tissue.
Other risk factors include:
- Advanced age, which reduces skin elasticity and resilience.
- Malnutrition, leading to weakened soft tissue and slower healing.
- Chronic conditions like heart disease or kidney failure, which impair overall health.
Impact of Underlying Comorbidities
Comorbidities play a significant role in the development of pressure-related wounds. For example, patients with diabetes often experience erythema and delayed wound healing due to poor circulation. Similarly, those with spinal cord injuries are at higher risk due to prolonged immobility.
Unique considerations are needed for patients with darker skin tones. Discoloration, such as purple or maroon hues, may be less visible, making early detection challenging. Clinicians must rely on tactile assessments and patient-reported symptoms to identify issues promptly.
The pressure ulcer advisory emphasizes the importance of regular assessments for at-risk patients. Early intervention, such as repositioning and using pressure-relieving devices, can prevent the progression to eschar or more severe complications.
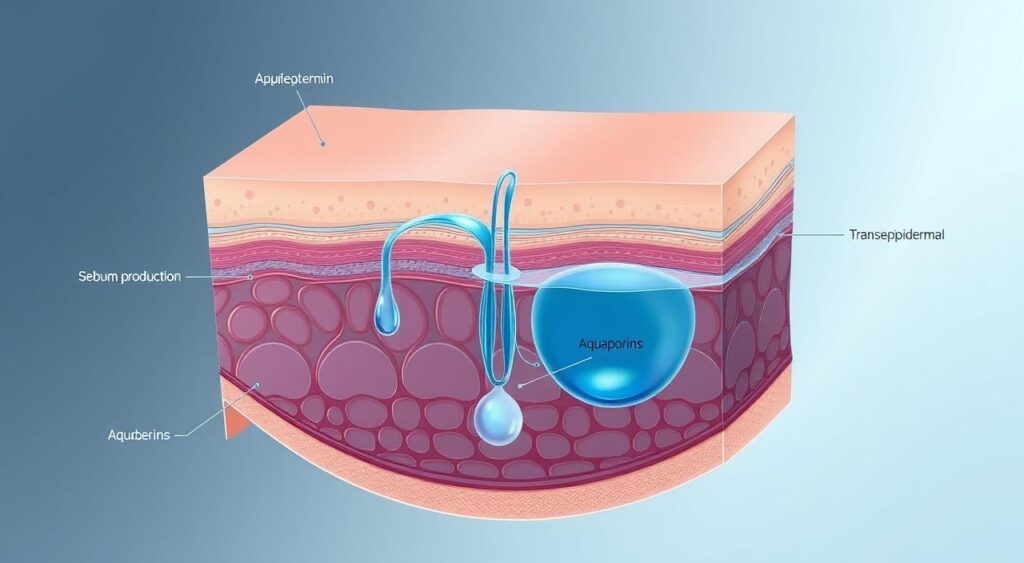
Causes and Mechanisms Behind Tissue Injury
The science behind pressure-related wounds reveals critical insights into their causes. Understanding the physical forces involved is essential for effective prevention and treatment. These mechanisms often lead to rapid deterioration if not addressed promptly.

Pressure and Shear Forces Explained
Intense pressure and shear forces are primary contributors to severe skin damage. When sustained, these forces compress blood vessels, reducing blood flow to the affected area. This lack of circulation can lead to ischemia, a condition where tissues are deprived of oxygen.
Shear forces, often caused by friction, exacerbate the problem by stretching and tearing soft tissue. This combination of pressure and shear can rapidly damage muscle fibers, making early intervention crucial. The ulcer advisory panel emphasizes the importance of recognizing these forces to prevent complications.
Ischemia, Necrosis, and the Role of Muscle Tissue
When ischemia persists, it can lead to necrosis, or tissue death. This process often begins in deeper layers, such as muscle, before becoming visible on the skin’s surface. Discoloration, such as maroon or purple hues, may signal underlying damage.
If left unaddressed, these injuries can evolve into full-thickness ulcers. The national pressure ulcer standards highlight the need for regular assessments to detect early signs. Patients with ostomy or similar conditions may face additional challenges, requiring tailored care plans.
By understanding these mechanisms, healthcare providers can implement strategies to reduce risks and improve outcomes. Early detection and proper management are key to preventing severe complications.
Diagnostic Approaches and Differential Diagnosis
Accurate diagnosis of pressure-related wounds requires a detailed and systematic approach. Clinicians must rely on advanced assessment techniques and a collaborative team effort to identify the condition correctly. Misdiagnosis can lead to ineffective treatment and worsen patient outcomes.
Comprehensive Wound Assessment Techniques
Thorough wound assessment is the cornerstone of accurate diagnosis. Clinicians often begin with visual inspection, looking for signs like non-blanchable erythema or discoloration. Palpation for induration and evaluation of blister formation are also critical steps.
Using guidelines from the ulcer advisory panel, healthcare providers can standardize their approach. These guidelines emphasize the importance of documenting wound characteristics, such as size, depth, and surrounding skin condition. This data helps in tracking progress and adjusting treatment plans.
Distinguishing Deep Tissue Injury from Similar Conditions
Differentiating pressure-related wounds from other skin conditions is essential. Conditions like skin tears, bruising, and dermatitis can mimic early signs of pressure damage. A team-based approach ensures a comprehensive evaluation, reducing the risk of misdiagnosis.
For example, skin tears often have irregular edges and are trauma-induced, unlike pressure-related wounds. The advisory panel recommends using diagnostic tools like ultrasound or MRI for deeper assessments. These tools provide a clearer picture of underlying tissue damage.
| Condition | Key Characteristics | Diagnostic Tools |
|---|---|---|
| Pressure-Related Wounds | Non-blanchable erythema, discoloration | Palpation, ultrasound |
| Skin Tears | Irregular edges, trauma-induced | Visual inspection |
| Bruising | Discoloration without defined borders | Patient history |
By following these methods, clinicians can ensure accurate diagnoses and improve patient care. Early detection and proper assessment are key to preventing complications and promoting recovery.
Treatment and Recovery Strategies
Effective treatment of pressure-related wounds requires a combination of conservative and advanced strategies. The purpose of these methods is to prevent further damage and promote healing. By following national guidelines and advisory recommendations, healthcare providers can ensure optimal patient outcomes.

Conservative Management and Offloading Techniques
Conservative treatment focuses on reducing pressure and improving blood flow. Offloading techniques, such as repositioning the patient every two hours, are essential. Specialized cushions and mattresses can also help distribute pressure evenly.
Moisture management is another critical aspect. Keeping the skin dry and clean prevents irritation and infection. Regular assessments ensure that any changes in the wound are addressed promptly.
Advanced Wound Care Options and Interventions
For more severe cases, advanced interventions may be necessary. Debridement removes dead tissue, promoting healthy healing. Moisture-retentive dressings maintain an optimal environment for recovery.
In cases of eschar, cautious management is crucial. The national pressure ulcer advisory panel recommends a tailored approach based on the wound’s stage and condition. Advanced therapies, such as negative pressure wound therapy, can also be effective.
By combining these strategies, healthcare providers can address tissue pressure injury effectively. Early intervention and adherence to guidelines are key to successful recovery.
Prevention and Early Intervention Techniques
Preventing severe skin damage starts with early intervention and effective pressure management. By addressing risks promptly, healthcare providers can reduce the likelihood of complications. This section explores proven strategies to safeguard skin health.
Best Practices in Pressure Redistribution
One of the most effective ways to prevent stage pressure injury is through proper pressure redistribution. Specialized mattresses and cushions help distribute weight evenly, reducing stress on vulnerable areas. Regular repositioning of patients is also critical to avoid prolonged pressure on any single spot.
Early identification of skin tears and superficial injuries is equally important. These minor issues can escalate into stage pressure ulcer if left untreated. Clinicians should conduct frequent skin assessments to catch problems before they worsen.
Here are some key prevention strategies:
- Use pressure-relieving devices like air mattresses or foam pads.
- Reposition patients every two hours to minimize pressure points.
- Keep skin clean and dry to prevent irritation and infection.
Specialized medical centers play a vital role in implementing these measures. Their wound care teams are trained to identify risks early and provide tailored solutions. Collaboration between caregivers and healthcare professionals ensures comprehensive care.
| Prevention Strategy | Implementation | Outcome |
|---|---|---|
| Pressure Redistribution | Use of specialized mattresses and cushions | Reduces risk of stage pressure injury |
| Regular Repositioning | Reposition patients every two hours | Minimizes prolonged pressure on skin |
| Skin Assessments | Frequent checks for skin tears and discoloration | Early detection of potential issues |
By following these evidence-based strategies, healthcare providers can significantly reduce the incidence of severe skin complications. Early intervention and proper care are the cornerstones of effective prevention.
Deep Tissue Injury: Essential Management and Pressure Injury Insights
Managing severe skin damage requires a proactive approach and adherence to proven guidelines. The National Pressure Ulcer Advisory Panel (NPUAP) provides critical standards for identifying and treating pressure-related wounds. These guidelines ensure that healthcare providers can deliver effective care and minimize complications.
Implementing National Pressure Ulcer Advisory Guidelines
Accurate stage assessment is the foundation of effective wound management. The NPUAP guidelines emphasize the importance of identifying the wound’s stage to determine the appropriate treatment plan. For example, early-stage wounds may require offloading techniques, while advanced cases might need debridement or advanced dressings.
Timely intervention is crucial to alter the clinical course of pressure injuries. As the NPUAP states,
“Early detection and proper management can prevent progression to severe complications.”
This approach reduces theriskof further tissue damage and improves patient outcomes.
Key components of the NPUAP guidelines include:
- Comprehensive wound area assessment to track progress and adjust treatment.
- Regular risk assessments to identify vulnerable patients.
- Implementation of pressure-redistribution devices to minimize risk.
Accurate wound area measurement is essential for monitoring healing. Clinicians use tools like digital imaging or wound tracing to document changes over time. This data helps tailor care plans and ensures that interventions are effective.
By following these evidence-based strategies, healthcare providers can significantly reduce the incidence of severe skin complications. Early intervention and proper care are the cornerstones of effective prevention.
Conclusion
This guide has explored the critical aspects of managing severe skin damage, from early detection to effective treatment. Recognizing signs like discoloration and changes in the wound bed is essential to prevent progression to necrosis. Timely intervention can halt further complications and promote healing.
Maintaining blood flow and monitoring muscle integrity are key to recovery. Proper care ensures that affected areas receive the nutrients needed for repair. Early action can significantly improve patient outcomes and reduce risks.
An integrated approach to wound care is vital. Combining prevention strategies, regular assessments, and advanced treatments offers the best chance for recovery. By staying vigilant and proactive, healthcare providers can make a meaningful difference in patient health.
FAQ
Q: What is deep tissue injury?
A: Deep tissue injury is a type of pressure ulcer that occurs beneath the skin’s surface, often affecting muscle and soft tissue. It can appear as a purple or maroon discoloration and may progress to necrosis if untreated.
Q: How can I identify early signs of this condition?
A: Early signs include persistent purple or maroon areas on the skin, localized pain, or changes in tissue texture. These visual indicators often precede more severe damage.
Q: Who is most at risk for developing this injury?
A: Patients with limited mobility, those with chronic illnesses like diabetes, and individuals with poor circulation are at higher risk. Comorbidities can further increase susceptibility.
Q: What causes deep tissue injury?
A: Prolonged pressure and shear forces disrupt blood flow, leading to ischemia and tissue death. Muscle tissue is particularly vulnerable to these forces.
Q: How is this condition diagnosed?
A: Diagnosis involves a thorough wound assessment, including visual inspection and palpation. It’s essential to differentiate it from other skin conditions like skin tears or stage pressure ulcers.
Q: What are the treatment options?
A: Treatment includes offloading pressure, using advanced wound care products, and monitoring the wound bed for changes. Severe cases may require surgical intervention.
Q: How can deep tissue injury be prevented?
A: Prevention focuses on pressure redistribution, regular skin checks, and following guidelines from the National Pressure Ulcer Advisory Panel. Early intervention is key.
Q: What role do the National Pressure Ulcer Advisory Panel guidelines play?
A: These guidelines provide evidence-based recommendations for prevention, assessment, and management of pressure injuries, including deep tissue injury.
Q: Can this condition lead to complications?
A: Yes, if untreated, it can progress to necrosis, infection, or even systemic issues. Prompt care is crucial to prevent complications.
Q: What should caregivers know about managing this condition?
A: Caregivers should be trained in wound care, recognize early signs, and ensure patients receive proper support to reduce pressure on vulnerable areas.
