Did you know 90% of women get menstrual cramps, with 10-20% feeling extreme pain? This is called dysmenorrhoea. It’s a common issue that affects women’s lives a lot. Knowing what causes it, its types, and how to treat it is key to better health.

Dysmenorrhoea, or menstrual cramps, is when the uterus contracts painfully during a woman’s period. It can be from mild to very severe. This pain can really get in the way of daily life and overall happiness.
In this article, we’ll explore dysmenorrhoea in detail. We’ll look at its causes, types, symptoms, and treatments. By the end, you’ll know a lot about this condition. This knowledge will help you manage your menstrual pain better.
Key Takeaways
- Dysmenorrhoea is a common gynecological condition affecting up to 90% of women, with 10-20% experiencing severe pain.
- It is characterized by painful uterine contractions during the menstrual period, ranging from mild discomfort to severe, debilitating pain.
- Understanding the causes, types, and risk factors of dysmenorrhoea is crucial for effective management and treatment.
- A combination of medical interventions, lifestyle changes, and natural remedies can help alleviate menstrual pain and improve quality of life.
- Seeking medical attention is recommended if menstrual pain is severe, persistent, or interferes with daily activities.
What is Dysmenorrhoea and Its Impact on Women’s Health
Dysmenorrhoea is a common condition in women, causing severe menstrual cramps. These cramps can greatly affect a woman’s life, making it hard to do daily tasks, work, and feel well.
About 50-90% of women of childbearing age deal with dysmenorrhoea. The pain can be mild or very severe, sometimes spreading to the back, belly, and thighs.
Dysmenorrhoea also affects a woman’s mind and feelings. The pain can make her stressed, anxious, and even depressed. This makes the condition’s impact on her health and daily life worse.
Many women suffer in silence, not knowing about treatments or being afraid to see a doctor. It’s important to address dysmenorrhoea and its causes. This helps women manage their menstrual health and feel better overall.
| Prevalence of Dysmenorrhoea | Impact on Daily Life |
|---|---|
| 50-90% of women of reproductive age | Interference with daily activities, work productivity, and overall well-being |
“Menstrual pain should not be considered a normal part of a woman’s life. It is a sign that something may be wrong and should be addressed.”
Primary vs Secondary Dysmenorrhoea: Key Differences
Dysmenorrhoea, or menstrual cramps, is divided into primary and secondary types. Knowing the differences between these two is key to managing and treating the pain effectively.
Characteristics of Primary Dysmenorrhoea
Primary dysmenorrhoea affects up to 90% of women during their reproductive years. It’s marked by sharp, cramping pain in the lower abdomen. This pain can spread to the lower back and thighs.
The pain usually starts before or at the beginning of the period. It can last for hours or even days.
Understanding Secondary Dysmenorrhoea
Secondary dysmenorrhoea is linked to health issues like endometriosis or uterine fibroids. This pain is often more intense and can get worse over time. Unlike primary dysmenorrhoea, it may not only occur during the period.
Age-Related Patterns and Onset
- Primary dysmenorrhoea often starts soon after the first period. It peaks in the late teens and early 20s.
- Secondary dysmenorrhoea can start at any age. It may begin later in life, sometimes decades after the first period.
It’s important for healthcare providers to know the differences between primary and secondary dysmenorrhoea. This helps them diagnose and treat menstrual cramps or pelvic pain accurately.
Common Symptoms and Warning Signs
Many women face menstrual pain, or dysmenorrhoea. It’s important to know the symptoms to find the right treatment.
Dysmenorrhoea often causes a dull, throbbing pain in the lower abdomen or pelvic area. This pain can spread to the lower back, thighs, or legs. The pain’s intensity can range from mild to very severe.
People with dysmenorrhoea might also feel:
- Nausea or vomiting
- Headaches or migraines
- Fatigue or dizziness
- Diarrhea or constipation
- Irritability or mood swings
It’s key to watch for warning signs of serious health issues. Severe, persistent menstrual pain or unusual bleeding needs medical help. These signs could point to problems like endometriosis, uterine fibroids, or pelvic inflammatory disease.
“Paying attention to the nature and severity of your menstrual pain can help you identify potential health concerns and take the necessary steps to address them.”

The Role of Hormones in Menstrual Pain
Dysmenorrhoea, or severe menstrual pain, is linked to hormones in the body. Knowing how hormones affect menstrual pain helps manage this condition better.
Prostaglandins and Pain Mechanisms
Prostaglandins, hormone-like substances, are key in uterine contractions. During menstruation, more prostaglandins are released. This leads to stronger uterine muscle activity and painful cramps, known as dysmenorrhoea.
Hormonal Imbalance Effects
Hormonal imbalances, especially in estrogen and progesterone, worsen menstrual pain. Too much or too little of these hormones can upset the body’s balance. This imbalance makes dysmenorrhoea symptoms more severe.
Endocrine System Involvement
The endocrine system controls hormone levels and distribution. It’s crucial in managing dysmenorrhoea. Problems in this system can cause hormonal changes, making menstrual pain worse.
Understanding the link between hormones and dysmenorrhoea helps doctors find better treatments. This can reduce menstrual pain and improve life quality for those with this condition.
Risk Factors Contributing to Dysmenorrhoea Diseases
Dysmenorrhoea, or severe menstrual cramps, can be influenced by many factors. Knowing these factors is key to managing and preventing the condition.
One big risk factor is genetic predisposition. Research shows that women with a family history of dysmenorrhoea are more likely to have it too. This points to a possible genetic link in menstrual pain.
Lifestyle choices also play a part. Sedentary behavior, poor diet, and high stress levels can lead to more cramps. On the other hand, staying active, eating well, and managing stress can help reduce the risk.
Certain medical conditions also raise the risk of dysmenorrhoea. Issues like endometriosis, uterine fibroids, and pelvic inflammatory disease can cause more severe pain.
| Risk Factor | Description |
|---|---|
| Genetic Predisposition | Hereditary factors that increase the risk of developing dysmenorrhoea |
| Lifestyle Factors | Sedentary behavior, poor diet, and high stress levels that contribute to menstrual pain |
| Medical Conditions | Endometriosis, uterine fibroids, and pelvic inflammatory disease associated with severe menstrual cramps |
By understanding these risk factors, women can take steps to improve their menstrual health. This can help lessen the impact of dysmenorrhoea on their life.
Medical Conditions Associated with Severe Menstrual Pain
Dysmenorrhoea, or severe menstrual pain, often stems from underlying medical issues. Three main conditions that can cause intense period discomfort are endometriosis, uterine fibroids, and pelvic inflammatory disease.
Endometriosis and Its Impact
Endometriosis is a chronic condition where endometrial tissue grows outside the uterus. This misplaced tissue reacts to hormonal changes, causing inflammation and scarring. These issues lead to severe menstrual cramps and pelvic pain.
Uterine Fibroids
Uterine fibroids are noncancerous growths in the uterine wall. Some women with fibroids have no symptoms, while others experience heavy, painful periods and pelvic pressure. The size, number, and location of fibroids affect the severity of pain.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. It’s often caused by sexually transmitted bacteria. PID can cause intense menstrual cramps, abdominal pain, fever, and abnormal vaginal discharge due to scarring and adhesions.
| Condition | Impact on Menstrual Pain | Key Symptoms |
|---|---|---|
| Endometriosis | Severe, debilitating cramps due to misplaced endometrial tissue | Pelvic pain, heavy bleeding, painful intercourse |
| Uterine Fibroids | Increased menstrual flow and pelvic pressure leading to cramps | Heavy, painful periods, pelvic pressure, enlarged uterus |
| Pelvic Inflammatory Disease | Scarring and adhesions causing intense menstrual cramps | Abdominal pain, fever, abnormal vaginal discharge |
It’s important to understand how these medical conditions affect menstrual pain. This knowledge helps in managing dysmenorrhoea and finding the right treatment.
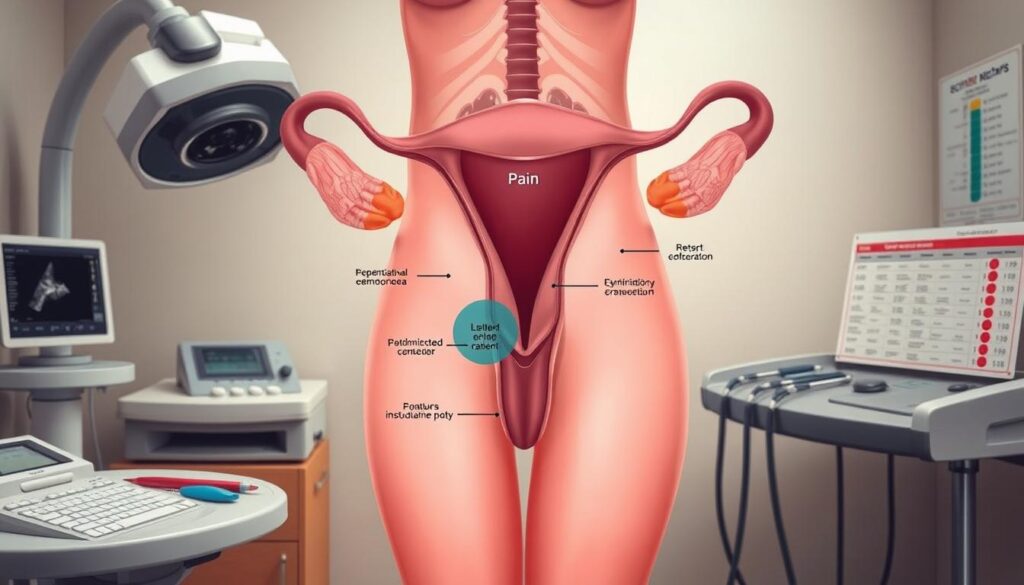
Diagnostic Approaches for Menstrual Pain
Finding the cause of severe menstrual pain is key to managing it well. Doctors use a detailed process to find out why women feel pelvic pain during their periods.
The first step is a thorough check-up. Doctors will look at your medical history and do a pelvic exam. They might also ask for more tests.
- Imaging techniques, such as ultrasound, MRI, or laparoscopy, to see if there are any problems like endometriosis or uterine fibroids.
- Laboratory tests, including blood work, to check for hormonal imbalances or other health issues.
- Pelvic pain assessment tools, like pain scales and questionnaires, to measure how bad the pain is.
Doctors use these methods together to understand the patient’s condition well. Then, they can create a treatment plan that fits the specific cause of the pain.
| Diagnostic Approach | Purpose |
|---|---|
| Physical Examination | Assess medical history, perform pelvic exam |
| Imaging Techniques | Visualize structural abnormalities (e.g., endometriosis, fibroids) |
| Laboratory Tests | Evaluate hormonal imbalances and underlying conditions |
| Pain Assessment Tools | Quantify the severity and impact of dysmenorrhoea |
Getting an accurate diagnosis helps doctors create a treatment plan. This plan aims to manage the causes of menstrual pain and help women find relief.
Modern Treatment Options and Pain Management
Healthcare professionals offer many ways to manage menstrual cramps, or dysmenorrhoea. These methods can be split into two main groups: medication and non-medication options. Each type aims to tackle the root causes and symptoms of this common issue.
Medication-Based Treatments
For mild to moderate pain, over-the-counter pain relievers like ibuprofen or naproxen are often recommended. These drugs help lessen prostaglandins, which cause uterine contractions and pain. For more severe cases, doctors might prescribe stronger options, such as hormonal birth control, to help manage the menstrual cycle and reduce cramps.
Non-Pharmacological Approaches
Those looking for alternative treatments have many options. These include:
- Heating pads or hot water bottles to soothe abdominal pain
- Acupuncture and acupressure techniques to stimulate specific pressure points
- Yoga, meditation, and other relaxation practices to manage stress and discomfort
- Dietary changes, such as increasing omega-3 fatty acids, to reduce inflammation
The right treatment depends on personal preferences, the severity of symptoms, and any health conditions. Working with healthcare providers, women can create a pain management plan that suits their needs. This plan can help manage menstrual cramps and improve their overall well-being.
| Treatment Option | Mechanism of Action | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) | Inhibit prostaglandin production | Moderate to high | Stomach discomfort, ulcers, increased bleeding |
| Hormonal Birth Control | Regulate menstrual cycle and reduce uterine contractions | High | Nausea, headaches, breast tenderness |
| Heating Pads | Improve blood flow and relax muscle tension | Moderate | Skin irritation, burns |
| Acupuncture | Stimulate pressure points to alleviate pain | Moderate to high | Minimal, such as minor bruising or soreness |
“Effective management of dysmenorrhoea requires a tailored approach that addresses the individual’s needs and preferences.”
Natural Remedies and Lifestyle Changes
If you’re dealing with menstrual pain, you’re not alone. Many women are trying natural remedies and lifestyle changes to feel better. These methods can help ease discomfort and improve overall health.
Herbal Remedies for Menstrual Pain
For centuries, herbs have helped with menstrual cramps. Some top natural remedies include:
- Ginger: It has anti-inflammatory properties that can reduce prostaglandins, causing less pain.
- Chamomile: This herb is calming and can help with pain and muscle relaxation.
- Cramp Bark: It relaxes the uterine muscles, offering relief from pain.
Dietary Modifications for Dysmenorrhoea
Changing your diet can also help with menstrual pain. Eating foods with omega-3 fatty acids is good. Avoiding processed foods, caffeine, and alcohol can also help.
Relaxation Techniques for Menstrual Pain Management
Stress can make menstrual pain worse. Relaxation techniques can help a lot. Some good methods include:
- Yoga and meditation: They reduce stress and relax the body, easing cramps.
- Warm baths: They relax muscles and ease discomfort.
- Massage therapy: Gentle massage on the abdomen and back can relieve tension and pain.
Exploring these natural remedies and lifestyle changes can help manage menstrual pain. It’s a proactive way to find relief.
| Natural Remedy | How It Helps |
|---|---|
| Ginger | Reduces prostaglandin production and inflammation |
| Chamomile | Has analgesic and antispasmodic effects to relieve cramps |
| Cramp Bark | Relaxes uterine muscles and provides pain relief |
By using these natural remedies and making lifestyle changes, women can manage their dysmenorrhoea and find relief from menstrual pain.
Understanding the Connection Between Diet and Menstrual Pain
Dysmenorrhoea, or severe menstrual pain, can really affect a woman’s life. New studies show that what we eat might help manage this pain. By learning how diet affects menstrual pain, women can take steps to feel better.
Anti-inflammatory Foods
Reducing inflammation is key to managing dysmenorrhoea. Some foods are great at fighting inflammation. These can be part of a diet that helps with menstrual pain. Here are some examples:
- Fatty fish, like salmon, mackerel, and sardines, are full of omega-3s.
- Turmeric, with its curcumin, is very anti-inflammatory.
- Ginger can cut down on prostaglandin and ease cramps.
- Leafy greens, like spinach and kale, are full of antioxidants and nutrients.
Nutrients for Pain Relief
Some nutrients are especially good for easing menstrual pain. These include:
- Magnesium helps relax the uterus and reduce cramps.
- Vitamin B1 (thiamine) helps lessen pain and discomfort.
- Calcium helps control muscle contractions and eases cramps.
- Omega-3s reduce inflammation and ease pain.
Adding these foods and nutrients to your diet can help a lot. Women with dysmenorrhoea might feel a lot less pain and discomfort.
“Making dietary changes can be a simple yet effective way for women to manage their menstrual pain and improve their overall quality of life.”
Exercise and Physical Activity Benefits
Adding regular exercise to your routine can help with dysmenorrhoea, or menstrual cramps. Studies show that different types of physical activity can lessen the pain of menstrual cramps. This can also boost your overall health.
Exercise is great for those with dysmenorrhoea because it reduces inflammation. Many menstrual cramps come from prostaglandins, which cause pain. By doing physical activities, you can lower these compounds and feel less pain.
- Low-impact exercises, such as walking, swimming, or gentle yoga, can be particularly beneficial in managing menstrual cramps.
- Aerobic activities, like jogging or cycling, can also help by increasing blood flow and endorphin production, which can have a natural pain-relieving effect.
- Strength training exercises, when done in moderation, can also contribute to a reduction in dysmenorrhoea symptoms.
It’s important to find activities that you enjoy and that work best for your individual needs. Try different exercises to see what helps your menstrual cramps the most. Being consistent is key, as the benefits of physical activity build up over time.
| Exercise Type | Benefits for Dysmenorrhoea |
|---|---|
| Low-Impact Exercises (e.g., walking, swimming, yoga) | Reduces inflammation and muscle tension, improves blood flow |
| Aerobic Activities (e.g., jogging, cycling) | Increases endorphin production, decreases pain perception |
| Strength Training | Helps stabilize the pelvic region and reduce muscle cramps |
Always talk to a healthcare professional before starting a new exercise routine, especially if you have severe or ongoing menstrual cramps. They can give you advice tailored to your needs and make sure the activities are safe and right for you.
“Regular exercise can be a game-changer in managing the symptoms of dysmenorrhoea. It’s a natural and effective way to reduce inflammation, ease muscle tension, and improve overall well-being.”
Mental Health and Dysmenorrhoea Management
Dysmenorrhoea, or severe menstrual pain, can really affect a woman’s mental health. Stress and anxiety can make symptoms worse, creating a tough cycle to get out of. But, by focusing on mental health, people can manage their pain better and live a better life.
Stress Reduction Techniques
Using stress reduction techniques daily can really help with dysmenorrhoea. Some good ways include:
- Practicing mindfulness meditation and deep breathing exercises
- Doing regular physical activity, like yoga or light exercise
- Setting time for relaxation and self-care, like a warm bath or reading
- Trying relaxation methods like progressive muscle relaxation or guided imagery
Psychological Support Methods
Getting psychological support is also key for those with dysmenorrhoea. Therapists and counselors offer a safe place to talk about feelings and find ways to cope. Helpful support methods include:
- Cognitive-behavioral therapy (CBT) to change negative thoughts and manage pain
- Support groups or networks to connect with others facing similar issues
- Mindfulness-based interventions to improve self-awareness and emotional control
- Relaxation techniques, such as guided visualization or progressive muscle relaxation
Combining stress reduction and psychological support can help manage dysmenorrhoea’s mental health aspects. This approach can greatly improve well-being and help deal with menstrual pain.
When to Seek Medical Help
Dysmenorrhoea, or severe menstrual pain, is common among women. Some pain during menstruation is normal. But, there are times when you should see a doctor. If you’re feeling any of these, it’s a good idea to talk to a healthcare professional:
- Persistent or worsening pelvic pain that interferes with your daily activities
- Menstrual cramps that are not relieved by over-the-counter pain medications
- Irregular menstrual cycles or significant changes in your flow
- Sudden or severe onset of menstrual pain, especially if it’s accompanied by other symptoms like nausea, vomiting, or diarrhea
- Pelvic pain that radiates to your lower back, thighs, or legs
- Bleeding between periods or after sexual intercourse
These signs might mean you have a problem like dysmenorrhoea, endometriosis, uterine fibroids, or pelvic inflammatory disease. Getting help early is key to managing these issues and avoiding bigger problems.
“Don’t hesitate to seek medical attention if your menstrual pain is significantly impacting your quality of life. Your healthcare provider can help determine the cause and develop an appropriate treatment plan.”
Listen to your body. If you’re worried about your menstrual health, speak up. With the right care and support, you can ease menstrual pain and pelvic pain. This will help you feel better overall.
Prevention Strategies and Long-term Management
Managing dysmenorrhoea, or menstrual cramps, needs a full plan. It covers both quick relief and long-term prevention. By using good prevention methods, women can lessen the effects of this common issue. This helps them live a better life.
Keeping reproductive health in check is key. Regular visits to the gynecologist and watching for any health problems are important. Treating issues like endometriosis or uterine fibroids can make menstrual pain less severe.
Living a healthy lifestyle is also vital. This means exercising regularly, eating well, and finding ways to reduce stress. By tackling both physical and emotional sides, women can control their pain better and feel better overall.
- Start regular physical activities like yoga, swimming, or low-impact aerobics. They help with menstrual cramps and improve pelvic and uterine health.
- Eat foods rich in omega-3 fatty acids, magnesium, and vitamins B1 and E. These nutrients help fight inflammation and lessen pain.
- Try relaxation methods like meditation, deep breathing, or guided imagery. They help manage stress and its effect on pain.
Women with ongoing or severe dysmenorrhoea should talk to a doctor. Doctors can offer tailored treatments, like medicine, hormonal therapy, or small procedures. These help find and fix the root causes and manage pain over time.
By using a mix of prevention strategies and getting medical help, women can manage their dysmenorrhoea. This improves their reproductive health and overall well-being.
Conclusion
Dysmenorrhoea, or menstrual pain, affects many women and can change their lives. We’ve looked at what causes it, its types, and how to treat it. We’ve also talked about ways to manage it on your own.
Good menstrual health is key. Women can manage their pain by making healthy choices and getting medical help when needed. There are many ways to feel better, from changing your diet to trying new treatments.
Managing dysmenorrhoea means women need to take charge of their health. They should learn about it and work with doctors to find the best treatments. By doing this, women can feel better and live a happier, more productive life.
FAQ
Q: What is dysmenorrhoea and how does it impact women’s health?
A: Dysmenorrhoea is severe or prolonged menstrual cramps and pelvic pain. It can disrupt a woman’s daily life, work, and overall well-being. It’s a common issue that affects many women, causing them to miss school or work and participate less in activities.
Q: What are the key differences between primary and secondary dysmenorrhoea?
A: Primary dysmenorrhoea is menstrual pain not caused by a medical condition. Secondary dysmenorrhoea is linked to conditions like endometriosis or uterine fibroids. Primary starts in adolescence, while secondary can occur at any age.
Q: What are the common symptoms and warning signs of dysmenorrhoea?
A: Symptoms include severe lower abdomen pain, back pain, nausea, vomiting, diarrhea, and fatigue. Warning signs include pain not helped by over-the-counter meds, worsening pain, and pain that affects daily life.
Q: How do hormones and the endocrine system contribute to menstrual pain?
A: Hormonal imbalances, especially too much prostaglandin, cause the uterus to contract too much. This leads to severe cramps and pain. The endocrine system, which controls hormone levels, is key in managing dysmenorrhoea.
Q: What are the common medical conditions associated with severe menstrual pain?
A: Conditions like endometriosis, uterine fibroids, and pelvic inflammatory disease can cause or worsen dysmenorrhoea. These can lead to chronic pain, heavy bleeding, and other symptoms that affect a woman’s life quality.
Q: What are the modern treatment options and pain management strategies for dysmenorrhoea?
A: Treatments include medications like pain relievers and hormonal therapies. Non-pharmacological methods include heat therapy, acupuncture, and lifestyle changes. It’s important to discuss treatment options with a healthcare provider for effective pain management.
Q: How can natural remedies and lifestyle changes help alleviate menstrual pain?
A: Eating anti-inflammatory foods, exercising regularly, and practicing stress-reduction techniques like meditation or yoga can help. Combining these natural approaches with medical treatment can effectively reduce menstrual pain and improve well-being.
Q: When should a woman seek medical help for severe menstrual pain?
A: Women should seek medical advice if pain isn’t helped by over-the-counter meds, interferes with daily life, or if they have other concerning symptoms like heavy bleeding or persistent pain.
