Did you know that about 20% of the world’s population deals with recurring mouth pain? This condition, known as glossitis-stomatitis, can make everyday tasks like eating and talking hard. It also affects how well you feel overall. Knowing what causes it and how to manage it is key to feeling better.
Key Takeaways
- Glossitis-stomatitis is a common mouth health issue, affecting 1 in 5 people globally.
- Finding out what’s causing it, like allergies or infections, is important for treatment.
- Simple home remedies and changes in your daily life can help. But, seeing a doctor is vital for serious cases.
- Keeping your mouth clean and using preventive measures are crucial for managing it long-term.
- If you have severe swelling, trouble swallowing, or other serious symptoms, get medical help right away.
Understanding Glossitis – stomatitis (sore mouth)
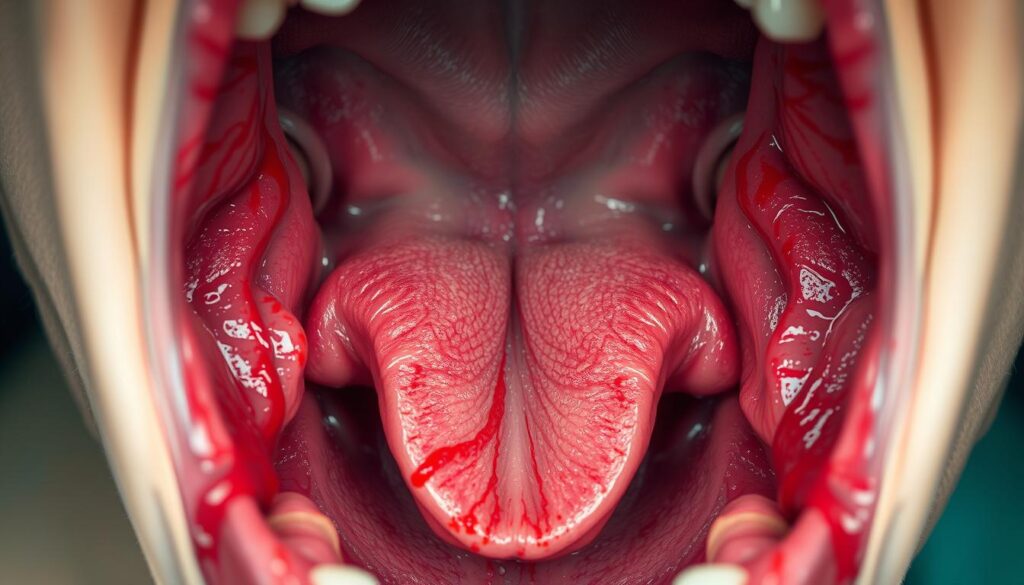
Glossitis and stomatitis are two related oral health issues. They cause discomfort and affect daily life. Symptoms include oral inflammation, tongue swelling, burning sensation, and tongue discoloration.
Common Symptoms and Signs
The main signs of glossitis-stomatitis are:
- Redness or inflammation of the tongue, lips, or entire mouth
- Tongue swelling or a burning sensation in the mouth
- Tongue discoloration, ranging from red to white or yellow patches
- Increased sensitivity to hot, cold, or spicy foods
- Difficulty swallowing or speaking due to discomfort
Impact on Daily Life
The symptoms of glossitis-stomatitis can greatly affect daily life. The oral inflammation and discomfort make eating, drinking, and speaking hard. This can lead to less nutrition, dehydration, and trouble with social interactions and communication.
When to Seek Medical Attention
If tongue swelling, burning sensation, or tongue discoloration lasts more than a few days, seek medical help. A healthcare professional can diagnose the cause and offer treatment. This helps to ease symptoms and prevent further problems.
Primary Causes of Oral Inflammation
Oral inflammation can lead to issues like oral thrush, dry mouth, and painful sores. It affects health and quality of life. Knowing what causes it is key to managing and preventing it.
Microbial infections are a big reason for oral inflammation. Candida fungus causes oral thrush, showing as white patches. Bacteria like Streptococcus or Staphylococcus can also cause pain and swelling.
Allergies to foods or the environment can also cause oral inflammation. Foods like gluten or dairy, or preservatives, can trigger an immune response. This leads to swelling, redness, and mouth discomfort.
| Cause | Symptoms | Risk Factors |
|---|---|---|
| Microbial Infections | Oral thrush Painful mouth sores Redness and swelling | Weakened immune system Antibiotic use Poor oral hygiene |
| Allergies and Sensitivities | Dry mouth Swelling and irritation Burning or tingling sensation | Genetic predisposition Exposure to allergens Weakened immune system |
It’s important to know what causes oral inflammation to treat it well. By tackling the main issues, people can find relief and avoid more problems.
The Connection Between Allergies and Mouth Sores
Allergies can cause mouth sores, also known as mouth ulcers or oral inflammation. Knowing how allergies and these painful conditions are linked can help manage symptoms and find relief.
Food Allergens
Certain foods, like mouth ulcers, can cause allergic reactions. This leads to oral inflammation and oral pain. Common allergens include citrus fruits, nuts, dairy, and spicy or acidic foods. People with food allergies often get mouth sores after eating these foods.
Environmental Triggers
Environmental factors also play a role in mouth sores. Irritants like harsh chemicals, medications, or new oral hygiene products can make the mouth lining inflamed and sensitive.
Cross-Reactive Substances
Some people’s immune systems react to substances as if they were allergens. This can happen with pollen, latex, or metals. It leads to allergic responses and mouth sores.
“Recognizing and avoiding the specific triggers that contribute to your mouth sores can be a significant step in managing your oral health.”
By finding and avoiding the allergens causing mouth sores, people can improve their oral health. This helps prevent and manage mouth sores, enhancing overall well-being.
Nutritional Deficiencies Leading to Oral Problems
Eating a balanced diet is key for our health, including our mouth and tongue. Some nutritional gaps can cause mouth and tongue issues. Knowing how diet affects our mouth health is the first step to solving these problems.
Vitamin B12 is vital for healthy mouth tissues. Not enough of it can cause glossitis, a swollen tongue. Iron deficiency can lead to atrophic glossitis, making the tongue look discolored and shiny.
- Vitamin B12 deficiency can cause glossitis, or swollen and inflamed tongue
- Iron deficiency may lead to atrophic glossitis, resulting in tongue discoloration and a smooth, shiny appearance
Zinc is also important for our mouth. Not enough zinc can cause mouth sores and inflammation. Eating foods rich in zinc or taking supplements can help prevent these issues.
To keep our mouths healthy, we need to eat foods full of vitamins and minerals. Eating fruits, vegetables, lean proteins, and whole grains helps our body get the nutrients it needs. This supports our oral health.
| Nutrient | Oral Health Impacts | Food Sources |
|---|---|---|
| Vitamin B12 | Glossitis (swollen, inflamed tongue) | Meat, poultry, eggs, dairy, fortified cereals |
| Iron | Atrophic glossitis (tongue discoloration and smooth appearance) | Red meat, spinach, lentils, fortified cereals |
| Zinc | Oral inflammation, canker sores | Oysters, red meat, poultry, beans, nuts |
By fixing nutritional gaps and eating a balanced diet, we can keep our mouths healthy. This helps prevent issues like oral inflammation, tongue swelling, and tongue discoloration.

Bacterial and Viral Infections Affecting Mouth Health
Our mouths can be affected by many bacterial and viral infections. These invaders can cause oral thrush, mouth ulcers, and oral inflammation.
Common Viral Infections
The herpes simplex virus (HSV) is a common problem for mouth health. It causes painful sores, known as cold sores or fever blisters. The varicella-zoster virus, which causes chickenpox, can also lead to shingles in the mouth. This results in blistering and discomfort.
Bacterial Complications
Bacterial infections, like streptococcal and staphylococcal bacteria, can cause oral thrush and oral inflammation. These can show up as white patches, redness, and a burning feeling in the mouth.
Prevention Methods
- Keep up with good oral hygiene by brushing, flossing, and using antiseptic mouthwashes regularly.
- Don’t share personal items like toothbrushes, utensils, and drinking glasses to stop infections from spreading.
- If you have persistent mouth ulcers or oral inflammation, see your healthcare provider.
Knowing about common viral and bacterial causes and keeping good oral health can help prevent these mouth problems.
Managing Tongue Swelling and Discomfort
Dealing with tongue swelling and oral discomfort from glossitis-stomatitis can be tough. But, there are many ways to find relief and feel better.
One quick fix is using cold compresses or ice packs on the sore area. This can help lessen swelling and ease burning sensation or oral pain. Also, a saltwater rinse can calm the irritated tissue and aid in healing.
For lasting relief, doctors might suggest over-the-counter corticosteroid creams or ointments. In serious cases, stronger meds or oral steroids might be needed.
Keeping your mouth clean is key during bad times. Use a soft-bristled toothbrush and avoid harsh mouthwashes. Eating cool foods like popsicles or ice cream can also help with tongue swelling and oral pain.
Sometimes, finding and fixing the cause of glossitis-stomatitis is important. This could be an allergy or a nutritional issue. Working with a healthcare provider is vital to create a treatment plan that works for you.
By using both quick fixes and long-term strategies, people with glossitis-stomatitis can manage tongue swelling and oral discomfort. This can greatly improve their life quality.
Effective Home Remedies for Oral Pain Relief
Dealing with oral pain, burning sensations, or dry mouth can be tough. But, there are home remedies that can help. These natural solutions and over-the-counter options can ease discomfort and aid in healing.
Natural Healing Solutions
Many things in your home can help with oral pain. A cold compress can reduce swelling and numb pain. Saltwater rinses can clean and soothe your mouth.
Chewing ice or sucking on popsicles can also offer quick relief. These methods can cool and numb your mouth.
Over-the-Counter Options
For quick relief, try over-the-counter meds. Topical anesthetics like lidocaine or benzocaine can numb the area. Oral pain relievers like acetaminophen or ibuprofen can also help.
Lifestyle Modifications
- Avoid foods and drinks that might make burning sensations or dry mouth worse. Stay away from spicy, acidic, or caffeinated items.
- Drink lots of water to keep your mouth moist and healthy.
- Brush and floss gently to avoid irritating your mouth further.
Using natural remedies, over-the-counter treatments, and making lifestyle changes can help. You can find relief from oral pain and aid in healing at home.
| Home Remedy | Description | Benefits |
|---|---|---|
| Cold Compress | Applying a cold, damp cloth or ice pack to the affected area | Reduces inflammation and provides numbing relief |
| Saltwater Rinse | Mixing a teaspoon of salt in a glass of warm water and swishing it around the mouth | Cleanses the mouth and soothes irritated tissues |
| Topical Anesthetic | Over-the-counter gels or ointments containing lidocaine or benzocaine | Temporarily numbs the painful area |
| Oral Pain Relievers | Acetaminophen or ibuprofen to reduce inflammation and discomfort | Alleviates overall oral pain and discomfort |
By using natural remedies, over-the-counter treatments, and making lifestyle changes, you can find relief from oral pain. You can heal at home.
Maintaining Proper Oral Hygiene During Flare-ups
Good oral hygiene is key when you have oral inflammation, like glossitis-stomatitis. Using gentle cleaning methods can help soothe sore mouths and aid in healing. It’s vital to be extra careful with your mouth when you have ulcers or discomfort.
During a flare-up, it’s important to avoid irritating your sensitive mouth tissues. Use a soft-bristled toothbrush and avoid scrubbing too hard. Choose toothpaste without harsh ingredients like sodium lauryl sulfate.
Also, rinsing with a mild, alcohol-free mouthwash can help. Look for mouthwashes with aloe vera or chamomile. These can help reduce inflammation.
- Use a soft-bristled toothbrush to gently clean teeth and gums
- Opt for a non-abrasive, gentle toothpaste
- Rinse with a mild, alcohol-free mouthwash to reduce oral inflammation
- Avoid flossing during active flare-ups to prevent further irritation
- Drink plenty of water to keep the mouth hydrated
By being gentle and careful with your oral care, you can manage your hygiene well. This helps reduce discomfort during glossitis-stomatitis flare-ups.
| Product | Key Features | Recommended for Oral Inflammation |
|---|---|---|
| Sensodyne Toothpaste | Designed for sensitive teeth, contains potassium nitrate | Yes |
| Biotene Mouthwash | Alcohol-free, contains soothing agents like xylitol and enzymes | Yes |
| Oral-B Sensitive Gum Care Toothbrush | Soft bristles, designed to clean gently | Yes |
By following these gentle oral hygiene practices, you can manage your oral health during inflammation or ulcers. This promotes healing and reduces discomfort.
Medical Treatments and Professional Care Options
If you have oral inflammation, tongue swelling, or oral thrush, you should see a doctor. They can suggest treatments to help you feel better. These treatments aim to reduce symptoms and find the cause.
Doctors might give you medicine to fight infections or reduce swelling. In some cases, they might need to do a biopsy or cauterization. This is to find and treat the problem.
Doctors also teach you how to take care of your mouth. They suggest changes in your daily routine to help you heal. Regular visits to the doctor are important to keep your mouth healthy.
Comprehensive Care Approach
Treating glossitis-stomatitis often means using many different methods. Doctors might give you medicine, do procedures, or suggest changes in your diet. They also want to see you regularly to check on your progress.
- Prescription medications, including topical corticosteroids, antifungal drugs, or antibiotics
- Specialized procedures, such as oral biopsies or cauterization, to diagnose and treat the underlying condition
- Dietary and lifestyle modifications to support healing and prevent future flare-ups
- Regular follow-up appointments to monitor progress and make necessary adjustments to the treatment plan
Working with your doctor helps you find the best treatment for your oral inflammation, tongue swelling, and other symptoms. This can greatly improve your oral health and overall well-being.
It’s very important to get medical help for any long-lasting or serious oral health problems. Early treatment can make a big difference in how well you recover.
Prevention Strategies and Long-term Management
Keeping your mouth clean is key to avoiding glossitis-stomatitis. This condition causes tongue and mouth inflammation. By taking the right steps, you can lower your risk and keep your mouth healthy for a long time.
Dietary Considerations
Eating a balanced diet full of nutrients is important. Foods like leafy greens, citrus fruits, and lean proteins help heal and prevent problems. They can also reduce the chance of getting sick again.
Lifestyle Changes
- Drink lots of water to fight dry mouth. It helps make saliva, which cleans your mouth.
- Stop smoking and drink less alcohol. These habits can make oral inflammation worse and slow healing.
- Manage stress with activities like meditation or yoga. Stress can weaken your immune system and harm your mouth.
Regular Check-ups
Seeing your dentist regularly is crucial. They can spot problems early and give you the right advice. This helps keep your mouth healthy and catches issues before they get worse.
| Prevention Strategies | Benefits |
|---|---|
| Maintain Proper Oral Hygiene | Reduces risk of inflammation and infection |
| Follow a Balanced Diet | Provides essential nutrients for healing and prevention |
| Lifestyle Modifications | Promotes overall oral and general health |
| Regular Dental Check-ups | Facilitates early detection and management of oral issues |
By using these prevention tips and managing your health long-term, you can lessen glossitis-stomatitis’s effects. This way, you can enjoy a healthier, more comfortable mouth.

When to Consider Emergency Care
Most oral pain, tongue swelling, or mouth ulcers can be treated at home. But, some cases need urgent medical help. Knowing when to seek emergency care is key to getting the right help fast.
If you have severe symptoms, get help right away. Here are some signs that mean you need emergency care:
- Sudden and severe swelling of the tongue or throat that makes it difficult to breathe or swallow
- Persistent and intense oral pain that does not respond to pain relief medications
- Uncontrolled bleeding from the mouth or tongue
- High fever accompanied by severe mouth or tongue pain
- Difficulty opening your mouth or moving your tongue due to stiffness or spasms
When you go to the emergency room, be ready to talk about your symptoms. Tell them how long you’ve had the pain, how bad it is, and what makes it better or worse. Also, share any health issues or medicines you’re taking. This info helps doctors treat you right away.
“Prompt medical attention is crucial when dealing with severe oral pain, tongue swelling, or mouth ulcers, as these symptoms can indicate a serious underlying condition that requires immediate intervention.”
Acting fast and getting professional help is very important. It can save your life. If you have any of these severe symptoms, don’t wait. Go to the emergency room or call emergency services right away.
Conclusion
In this guide, we’ve looked closely at . We’ve covered its causes, how it affects daily life, and why getting medical help quickly is crucial. We’ve also talked about how allergies and nutritional gaps can cause mouth sores.
Keeping up with and using home remedies for pain are key. Also, getting professional help and following prevention tips are vital. This includes watching what you eat and going for regular dental check-ups.
Being proactive and acting fast is important for dealing with . By staying informed and working with doctors, you can improve your oral health. This leads to a more comfortable and confident life. Take care of your mouth today and start a journey to better oral health.
FAQ
Q: What is glossitis – stomatitis (sore mouth)?
A: Glossitis-stomatitis is a painful mouth and tongue condition. It causes inflammation, swelling, and discomfort.
Q: What are the common symptoms of glossitis – stomatitis?
A: Symptoms include tongue swelling, oral pain, and a burning sensation. You might also see mouth ulcers and tongue discoloration.
Q: How does glossitis – stomatitis impact daily life?
A: It makes eating, drinking, and speaking hard. The mouth’s discomfort and sensitivity hinder daily activities.
Q: When should someone seek medical attention for glossitis – stomatitis?
A: See a doctor if symptoms don’t get better, get worse, or affect your daily life. Look out for signs of infection or severe swelling.
Q: What are the primary causes of oral inflammation in glossitis – stomatitis?
A: Inflammation can come from infections, allergies, nutritional deficiencies, and certain diseases.
Q: How are allergies related to mouth sores in glossitis – stomatitis?
A: Food allergens, environmental triggers, and cross-reactive substances can cause mouth sores and inflammation.
Q: Can nutritional deficiencies lead to oral problems in glossitis – stomatitis?
A: Yes, lacking certain vitamins and minerals can lead to tongue swelling and discoloration, among other oral issues.
Q: What types of bacterial and viral infections can affect mouth health in glossitis – stomatitis?
A: Oral thrush (candidiasis) and herpes simplex virus are common infections. They can make mouth sores and inflammation worse.
Q: How can tongue swelling and discomfort be managed in glossitis – stomatitis?
A: Topical medications, anti-inflammatory drugs, and home remedies can help with tongue swelling and discomfort.
Q: What are some effective home remedies for oral pain relief in glossitis – stomatitis?
A: Natural solutions, over-the-counter options, and lifestyle changes can help with oral pain and discomfort.
Q: How can proper oral hygiene be maintained during glossitis – stomatitis flare-ups?
A: Use gentle cleaning techniques and suitable oral hygiene products. This helps manage inflammation and maintain good oral health.
Q: What medical treatments and professional care options are available for glossitis – stomatitis?
A: Healthcare providers might suggest prescription medications, topical treatments, or procedures for severe cases.
Q: How can glossitis – stomatitis be prevented and managed in the long term?
A: Eat a healthy diet, make lifestyle changes, and visit your dentist regularly. These steps can help prevent and manage glossitis-stomatitis.
Q: When should someone seek emergency care for glossitis – stomatitis?
A: Get emergency help if you have severe swelling, trouble breathing or swallowing, or other life-threatening symptoms.
