The World Health Organization says intestinal tuberculosis (ITB) makes up to 15% of all TB outside the lungs worldwide. This serious TB form hits the gut, making it a big health problem, especially in poor countries. Knowing the signs, how to find it, and how to treat it is key for doctors and patients. Early action and right treatment can really help.
This guide dives deep into intestinal tuberculosis. It covers what it is, why it happens, its symptoms, how to find it, and new ways to treat it. If you’re a doctor wanting to learn more or someone worried about this disease, this article has the info you need to understand intestinal tuberculosis better.

Key Takeaways
- Intestinal tuberculosis is a severe form of extrapulmonary TB that affects the gastrointestinal tract.
- It accounts for up to 15% of all extrapulmonary TB cases globally, posing a significant public health concern.
- Early diagnosis and appropriate treatment are crucial for improving patient outcomes.
- Understanding the symptoms, diagnostic methods, and treatment options is essential for healthcare providers and patients.
- Comprehensive management of intestinal TB requires a multidisciplinary approach, including medical, surgical, and nutritional interventions.
Understanding Intestinal Tuberculosis: Definition and Overview
Intestinal tuberculosis, also known as bowel tuberculosis or tuberculous enteritis, is a rare form of tuberculosis (TB) that affects the digestive system. It is caused by the bacterium Mycobacterium tuberculosis, which can move from the lungs to the digestive system. This serious illness needs quick diagnosis and proper treatment to save lives.
Types of Gastrointestinal TB
There are several types of gastrointestinal TB, including:
- Ileocecal TB: This is the most common type, affecting the terminal ileum and cecum of the small intestine.
- Colonic TB: This form primarily involves the colon, often leading to strictures and obstruction.
- Peritoneal TB: In this type, the tuberculous infection affects the peritoneum, the membrane lining the abdominal cavity.
Global Prevalence and Risk Factors
Intestinal tuberculosis is more common in developing countries. It is linked to poverty, malnutrition, and weakened immune systems. People with HIV/AIDS are at higher risk. Other factors include a history of TB, long-term steroid use, and certain digestive disorders.
| Region | Prevalence of Intestinal TB |
|---|---|
| Asia | High |
| Africa | High |
| Latin America | Moderate |
| North America and Europe | Low |
The global prevalence of intestinal tuberculosis shows the need for better awareness and management. Early detection and effective treatment are crucial to fight this serious disease.
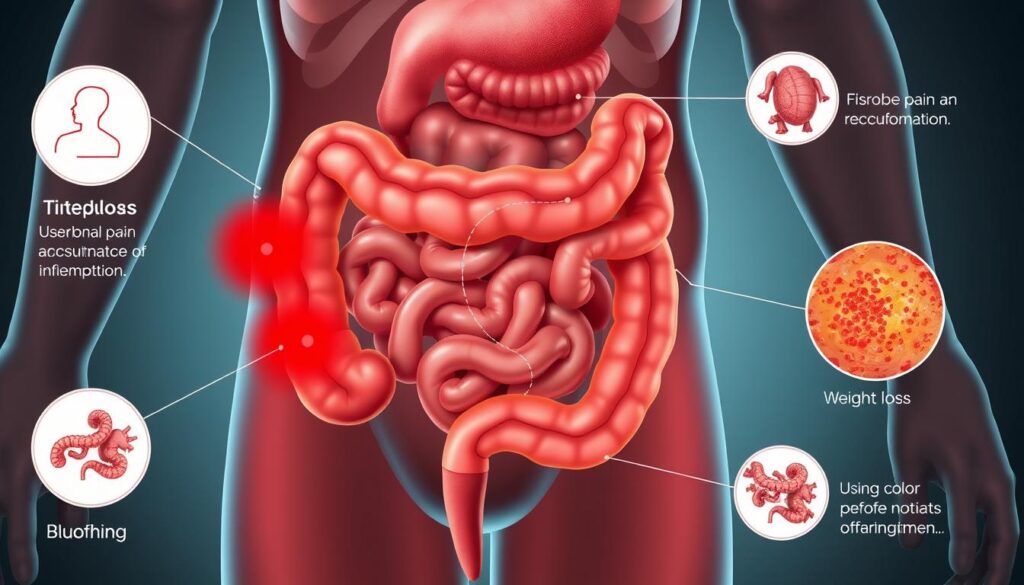
Common Symptoms of Bowel Tuberculosis
It’s important to spot the early signs of intestinal tuberculosis. This type of abdominal tuberculosis can cause many different symptoms. These symptoms might not seem related to the infection at first.
Abdominal pain is a common symptom. It can feel dull, cramping, or colicky. People may also lose weight and have fever as their body fights the infection. Changes in bowel habits, like diarrhea or constipation, are also common.
- Abdominal pain and discomfort
- Unintentional weight loss
- Persistent fever
- Altered bowel movements (diarrhea, constipation, or alternating)
- Fatigue and malaise
- Nausea and vomiting
- Abdominal distension or bloating
These intestinal tuberculosis symptoms can look like other stomach problems. This makes it hard to get a correct diagnosis. It’s key to see a doctor regularly and report any ongoing or worrying stomach issues. This helps catch abdominal tb signs early and manage them properly.
“Early recognition of intestinal tuberculosis symptoms is key to initiating timely and appropriate treatment, ultimately improving patient outcomes.”
Pathophysiology of Intestinal TB Infection
Intestinal tuberculosis is a complex disease caused by mycobacterium tuberculosis. It affects the digestive system. Knowing how it works is key to diagnosing and treating it effectively.
How Mycobacterium Tuberculosis Affects the Digestive System
The bacteria can enter the body through the lungs and reach the digestive tract. There, it causes intestinal granulomas. These are areas of inflammation and damage from the immune system’s fight against the infection.
These granulomas can disrupt the digestive system’s normal function. Symptoms and complications can arise. As the disease worsens, the granulomas can lead to ulcers, damaging the intestinal lining. This can cause blockages, perforations, or fistulas.
Disease Progression Stages
The progression of intestinal tuberculosis can be broken down into stages:
- Initial infection: The bacteria start to grow in the digestive system.
- Granuloma formation: The immune system forms granulomas in the intestines.
- Ulceration and tissue damage: The granulomas can ulcerate, causing more damage to the intestinal lining.
- Fibrosis and scarring: The body tries to heal, leading to fibrosis and scarring. This can cause blockages or other complications.
Understanding intestinal tuberculosis is crucial for healthcare professionals. It helps them provide the right treatment. This improves patient outcomes and reduces the risk of long-term problems.
Risk Factors and High-Risk Populations
Intestinal tuberculosis, or gastrointestinal tuberculosis, is a serious health issue that affects the digestive system. It’s important to know the risk factors and who is most at risk. This helps in early detection and prevention.
A weakened immune system, often seen in HIV/AIDS, is a major risk factor. People with HIV are more likely to get gastrointestinal tuberculosis because their immune system can’t fight off infections well. Malnutrition and other conditions that weaken the immune system also increase the risk.
- Weakened immune system (e.g., HIV/AIDS)
- Malnutrition and undernutrition
- Immunosuppressive medications or treatments
Places with high tuberculosis rates, especially in developing countries, are at higher risk for intestinal tuberculosis. Poor healthcare access, bad sanitation, and crowded living conditions make it easier for the bacteria to spread.
| High-Risk Regions | Prevalence Rates |
|---|---|
| Sub-Saharan Africa | 60-80 cases per 100,000 population |
| Southeast Asia | 45-60 cases per 100,000 population |
| Central Asia | 40-55 cases per 100,000 population |
Knowing the risk factors and who is most at risk helps healthcare professionals. They can then focus on preventive measures and early treatment to reduce the impact of intestinal tuberculosis.
“Recognizing the risk factors and vulnerable populations is the first step in addressing the burden of intestinal tuberculosis worldwide.”
Diagnostic Methods for Intestinal Tuberculosis
Diagnosing intestinal tuberculosis (TB) can be tricky. Symptoms often look like other stomach problems. But finding it right and fast is key for good treatment. Let’s look at how doctors spot abdominal TB.
Imaging Techniques
Imaging is a big help in finding intestinal TB. Computed Tomography (CT) scans show detailed pictures of the stomach area. They can spot thickened walls, big lymph nodes, and other signs of TB.
Magnetic Resonance Imaging (MRI) is used too. It helps see how far the disease has spread, especially in the belly area.
Laboratory Tests and Procedures
Lab tests and procedures are also used to find TB in the gut. Stool cultures and polymerase chain reaction (PCR) assays check for TB bacteria. Endoscopic examinations let doctors see inside and take tissue samples for tests.
Using all these methods, along with a patient’s history and physical check-up, helps doctors find TB. This way, they can tell it apart from other stomach issues like Crohn’s disease or cancer.
“Early and accurate diagnosis of intestinal tuberculosis is essential for timely initiation of appropriate treatment, which can significantly improve patient outcomes.”
Clinical Manifestations and Complications
Intestinal tuberculosis (TB) shows many symptoms, both local and widespread. Knowing the bowel tuberculosis complications and intestinal tb manifestations is key for quick diagnosis and treatment.
Abdominal pain is a common symptom, with varying intensity and location. Changes in bowel habits, like diarrhea or constipation, are also common. Gastrointestinal bleeding and weight loss are often seen in intestinal TB patients.
- Intestinal obstruction: Thickening of the bowel wall or the development of intestinal strictures can lead to partial or complete obstruction, causing nausea, vomiting, and abdominal distension.
- Intestinal perforation: In severe cases, the weakened intestinal wall may perforate, leading to life-threatening complications like peritonitis and sepsis.
- Fistula formation: Intestinal TB can result in the development of abnormal connections (fistulas) between the bowel and other organs, such as the bladder or the skin, causing further complications.
Systemic symptoms include fever, night sweats, and malaise, showing the body’s fight against the infection. Some may also have extraintestinal tuberculosis, like lung TB or swollen lymph nodes.
| Clinical Manifestation | Prevalence |
|---|---|
| Abdominal pain | 60-90% |
| Diarrhea/Constipation | 40-80% |
| Gastrointestinal bleeding | 20-50% |
| Weight loss | 50-80% |
| Intestinal obstruction | 15-40% |
| Intestinal perforation | 5-15% |
| Fistula formation | 10-20% |
The variety of intestinal tb manifestations and bowel tuberculosis complications highlights the need for thorough evaluation. It’s crucial to suspect intestinal TB, especially in high-risk groups and areas where TB is common.

Differential Diagnosis: Distinguishing from Other Conditions
Diagnosing intestinal tuberculosis (TB) is tricky because its symptoms can look like other gut problems. Doctors must figure out if it’s TB or something else like Crohn’s disease, ulcerative colitis, or gastrointestinal malignancies. This is to make sure they treat it right.
Similar Conditions and Their Characteristics
To tell intestinal TB apart from other gut issues, it’s important to know their differences:
- Crohn’s disease has deep inflammation, skip lesions, and problems in the anus. Intestinal TB usually has more focused inflammation and ulcers.
- Ulcerative colitis causes ongoing inflammation that starts in the rectum. TB lesions are more patchy and don’t always start there.
- Gastrointestinal malignancies might look like TB with their growths. But they often cause weight loss, hunger loss, and can block or burst.
Key Diagnostic Indicators
To spot intestinal tuberculosis, doctors look for certain signs:
- Seeing extra-intestinal tuberculosis like lung or lymph node TB
- Seeing ulcers, strictures, and swollen lymph nodes in endoscopic and imaging studies
- Getting a positive tuberculosis bacteriology test, like finding acid-fast bacilli
- Seeing the disease get better with anti-tuberculosis treatment
It’s key to correctly identify intestinal TB to manage it well and avoid gastrointestinal tb misdiagnosis. Doctors use a mix of patient history, imaging, and lab tests to make the right call.
Treatment Options and Medical Management
Treating intestinal tuberculosis needs a detailed and personalized plan. The main goal is to get rid of the Mycobacterium tuberculosis infection and ease symptoms. A team of doctors, including gastroenterologists and infectious disease specialists, works together to create a treatment plan.
The key to treating intestinal tuberculosis is using anti-tubercular medicines. These medicines, often a mix of four drugs, are taken for 6 to 9 months. The treatment plan is made just for the patient, considering things like drug resistance and how severe the disease is.
Supportive care is also very important in managing intestinal tuberculosis. This includes giving nutrients, managing fluids and electrolytes, and helping with symptoms. Sometimes, surgery is needed to fix problems like blockages or holes in the intestines.
Success in treating intestinal tuberculosis depends on early diagnosis and starting treatment quickly. Regular check-ups and tests are key to making sure the treatment is working and to catch any problems early.
Treating intestinal tuberculosis is a complex task. It involves medical treatment, supportive care, and sometimes surgery. By focusing on the infection and supporting the patient’s health, doctors can help people with intestinal tuberculosis get better and live a better life.
Medication Protocols and Duration
Effective treatment for intestinal tuberculosis needs a well-planned medication plan. The main drugs for gastrointestinal tb are isoniazid, rifampicin, ethambutol, and pyrazinamide.
First-Line Drugs
- Isoniazid – This key drug targets the Mycobacterium tuberculosis bacteria. It stops their cell wall synthesis and growth.
- Rifampicin – A strong antibiotic that stops bacterial RNA synthesis. This effectively kills the tuberculosis pathogen.
- Ethambutol – It helps prevent drug resistance by affecting the bacterial cell wall construction.
- Pyrazinamide – This drug acidifies the bacterial environment. This makes it hard for tuberculosis bacteria to survive.
Treatment Timeline and Monitoring
The usual treatment for intestinal tuberculosis medication lasts 6 to 12 months. This depends on the patient’s response and the infection’s severity. Regular checks through clinical assessments, imaging, and lab tests are key. They help track progress and ensure the gastrointestinal tb drug therapy is working.
“Timely and consistent administration of the prescribed medications is essential for achieving a successful outcome in the management of intestinal tuberculosis.”
Surgical Interventions and Indications
Sometimes, surgery is needed to treat intestinal tuberculosis. This is when medicine alone can’t help or when complications arise.
The main surgeries for intestinal tuberculosis are:
- Removing damaged bowel parts: If the disease has harmed the intestines a lot, surgeons might take out the bad parts.
- Draining abscesses: Abscesses in the belly, a common problem, need to be drained to ease pressure and avoid more issues.
- Fixing fistulas: Fistulas, or abnormal connections, need surgery to fix them.
Choosing surgery depends on how sick the person is, how bad the disease is, and if medicine helped. Doctors look at the risks and benefits to help the patient the most.
| Surgical Procedure | Indication | Potential Outcomes |
|---|---|---|
| Resection of affected bowel segments | Severe intestinal damage or obstruction | Improved intestinal function, reduction of complications |
| Drainage of abscesses | Localized abdominal abscesses | Alleviation of pressure, prevention of further complications |
| Fistula repair | Abnormal connections between the intestines and other organs | Restoration of normal intestinal anatomy, improved quality of life |
Surgery is usually a last choice but is key for managing serious intestinal tuberculosis cases. Patients should talk to their doctors about the risks and benefits to decide on treatment.
Dietary Recommendations and Nutritional Support
Proper nutrition is key for those with intestinal tuberculosis to recover well. A balanced diet with essential nutrients helps the body heal. It also makes treatment more effective.
Essential Nutrients for Recovery
When treating gastrointestinal tb, it’s important to eat foods rich in certain nutrients:
- Protein: Found in lean meats, eggs, dairy, and legumes, protein helps rebuild and repair damaged tissues.
- Vitamins A, C, and E: These antioxidants support the immune system and fight inflammation.
- Zinc: This mineral is essential for wound healing and immune function.
- Iron: Adequate iron intake helps prevent anemia, a common complication of intestinal tuberculosis.
Foods to Avoid During Treatment
It’s also important to limit or avoid certain foods that can hinder treatment or worsen symptoms:
- Spicy and fried foods: These can irritate the digestive tract and worsen gastrointestinal discomfort.
- Alcohol and caffeine: Both can impede nutrient absorption and medication effectiveness.
- High-fiber foods: During active infection, high-fiber items may cause further irritation and discomfort.
By following a targeted intestinal tuberculosis diet and seeking professional nutritional guidance, individuals with gastrointestinal tb can support their recovery and overall well-being.
Remember, the specific dietary needs may vary depending on the individual’s condition and stage of treatment. It is essential to work closely with healthcare providers to develop a personalized nutrition plan that addresses the unique requirements of each patient.
Prevention Strategies and Risk Reduction
Preventing intestinal tuberculosis (TB) and reducing the risk of abdominal TB are key steps. Several strategies can help protect against this disease. They also help prevent its development.
Vaccination and Immune System Support
The BCG (Bacille Calmette-Guérin) vaccine is a major prevention method. It offers some protection against intestinal tuberculosis prevention. A healthy lifestyle, balanced diet, and regular exercise also boost the immune system. This helps fight off abdominal tb risk reduction.
Early Detection and Treatment of Pulmonary TB
Intestinal TB often comes from pulmonary TB. Early treatment of lung TB can greatly reduce the risk of it spreading to the digestive system. Regular screenings and quick medical action are essential.
| Prevention Strategy | Potential Impact |
|---|---|
| BCG Vaccination | Provides some protection against intestinal TB |
| Maintaining Immune Health | Strengthens the body’s defenses against abdominal TB |
| Early Pulmonary TB Detection | Reduces the risk of intestinal TB development |
By using these prevention strategies and tackling risk factors, we can fight intestinal tuberculosis. This helps improve health outcomes for individuals and communities.
“Early detection and treatment of pulmonary TB is crucial in preventing the spread of the disease to the digestive system.”
Recovery Process and Follow-up Care
Getting better from intestinal tuberculosis needs a full plan. This includes sticking to treatment and regular check-ups. It’s a tough journey, but with the right help, patients can get back to their lives.
Monitoring Progress
It’s key to have regular visits and tests during intestinal tuberculosis recovery. Doctors will use CT scans or endoscopies to see how healing is going. Blood tests might also be done to check for certain markers.
Patients will also meet with their doctors to talk about how they’re feeling. They’ll discuss any ongoing symptoms and how well the gastrointestinal tb follow-up plan is working.
Long-term Management Strategies
- Continued medication adherence: Patients must finish all the anti-tuberculosis drugs, even if symptoms go away. This helps avoid relapse.
- Lifestyle modifications: Eating well, exercising, and managing stress can help recovery and prevent future problems.
- Ongoing monitoring: Regular visits and checks for any signs of coming back or long-term issues are important, even after treatment ends.
By working with their healthcare team and sticking to the intestinal tuberculosis recovery plan, patients can heal. This helps reduce the chance of lasting problems.
“The key to successful recovery from intestinal tuberculosis is a combination of strict adherence to treatment and a commitment to long-term management strategies.”
Living with Intestinal TB: Lifestyle Modifications
Living with intestinal tuberculosis, or bowel TB, comes with its own set of challenges. But, with the right lifestyle changes, patients can feel better and manage their condition more effectively.
Managing stress is key when living with intestinal TB. This disease can make you feel anxious, depressed, and isolated. Activities like meditation, yoga, or deep breathing can help you deal with these feelings.
- Practice mindfulness techniques to promote relaxation and mental well-being.
- Engage in regular physical activity, such as light exercises or gentle walks, to boost mood and energy levels.
- Seek support from a counselor or join a support group to connect with others facing similar challenges.
Along with stress management, bowel TB lifestyle changes should also include a healthy diet and staying active. Eating a balanced diet rich in nutrients can help your body recover and support your immune system. It’s important to work with your healthcare team to create a diet plan that meets your needs.
| Recommended Foods | Foods to Avoid |
|---|---|
| Fruits, vegetables, whole grains, lean proteins, and probiotic-rich foods | Spicy, fried, or heavily processed foods, as well as foods that may aggravate digestive symptoms |
By adopting these lifestyle changes, people with intestinal tuberculosis can play an active role in their recovery. This can greatly improve their quality of life.
“Embracing a holistic approach to living with intestinal TB can empower patients and help them navigate the challenges of this condition with resilience and hope.”
Conclusion
Intestinal tuberculosis is a complex and often overlooked condition. It needs comprehensive management and ongoing research to improve patient outcomes. Early diagnosis, targeted treatment, and a holistic approach to care are key in tackling this form of gastrointestinal TB.
Healthcare providers must stay alert to the diverse symptoms. They should use advanced diagnostic tools for timely intervention. This ensures better care for those affected.
Raising awareness and understanding of intestinal tuberculosis is crucial. Collaborations between medical professionals, public health organizations, and the scientific community are vital. They drive innovative treatment strategies and improve the quality of life for those affected.
Through a collective effort, we can work towards eradicating the burden of intestinal tuberculosis. Ensuring individuals worldwide receive comprehensive care and support is essential. By prioritizing intestinal tuberculosis management and gastrointestinal TB awareness, we can pave the way for a healthier future for all.
FAQ
Q: What is intestinal tuberculosis?
A: Intestinal tuberculosis is a serious form of tuberculosis that affects the gut. It’s caused by Mycobacterium tuberculosis. If not treated, it can cause serious problems.
Q: What are the common symptoms of intestinal tuberculosis?
A: Symptoms include stomach pain, weight loss, and fever. You might also have changes in bowel habits or bleeding. Fatigue, nausea, and loss of appetite are common too.
Q: How is intestinal tuberculosis diagnosed?
A: Doctors use CT scans and MRIs to diagnose it. They also do stool cultures and PCR assays. Colonoscopy helps them look at the gut and take tissue samples.
Q: What are the treatment options for intestinal tuberculosis?
A: Treatment involves taking several medicines for 6 to 12 months. These include isoniazid and rifampicin. Sometimes, surgery is needed to fix complications like blockages or holes in the gut.
Q: What are the risk factors for developing intestinal tuberculosis?
A: Risk factors include HIV/AIDS and poor nutrition. People in areas with lots of tuberculosis are also at higher risk.
Q: How can intestinal tuberculosis be prevented?
A: Early treatment of lung TB and vaccination help prevent it. Eating well and staying healthy also helps. Good hygiene and avoiding sick people can reduce risk.
Q: What is the recovery process for patients with intestinal tuberculosis?
A: Recovery means sticking to the treatment plan and regular check-ups. This helps manage side effects and prevent the disease from coming back. A healthy lifestyle and regular health checks are key.
