About 5 people in every 100,000 get intracranial venous thrombosis each year. It’s a rare but serious condition that needs attention. A blood clot forms in the brain’s veins, leading to severe problems if not treated.
It’s important to know about intracranial venous thrombosis. This way, you can spot its signs and symptoms early. You can also take steps to lower your risk of getting it.
Knowing about intracranial venous thrombosis helps keep your brain healthy. It can greatly affect your life quality. So, learning about its causes, symptoms, and treatments is key.
By understanding the risks and effects of intracranial venous thrombosis, you can protect your brain. This reduces the chance of getting this condition.
Key Takeaways
- Intracranial venous thrombosis is a rare but serious condition that affects 5 people out of 100,000 each year.
- Understanding intracranial venous thrombosis is essential for recognizing its signs and symptoms and taking preventive measures.
- Intracranial venous thrombosis can have a significant impact on a person’s quality of life.
- Being informed about intracranial venous thrombosis can help individuals take proactive steps to protect their brain health.
- Intracranial venous thrombosis requires attention and understanding to reduce the risk of developing this condition.
Understanding Intracranial Venous Thrombosis
Intracranial venous thrombosis is when a blood clot forms in the brain’s veins. This can cause serious problems if not treated. It’s a form of venous thrombosis that affects the brain’s veins.
The brain’s venous system is complex. Venous thrombosis can happen in different parts. There are several types, each needing its own treatment.
Definition and Basic Concepts
Venous thrombosis happens when a blood clot forms in veins. It can be caused by many things like injury or infection. In intracranial venous thrombosis, the clot forms in brain veins. This can lead to high pressure and serious problems.
Types of Cerebral Venous Thrombosis
There are two main types of cerebral venous thrombosis. One is in the deep veins of the brain. The other is in the superficial veins. Each type has its own characteristics and treatment.
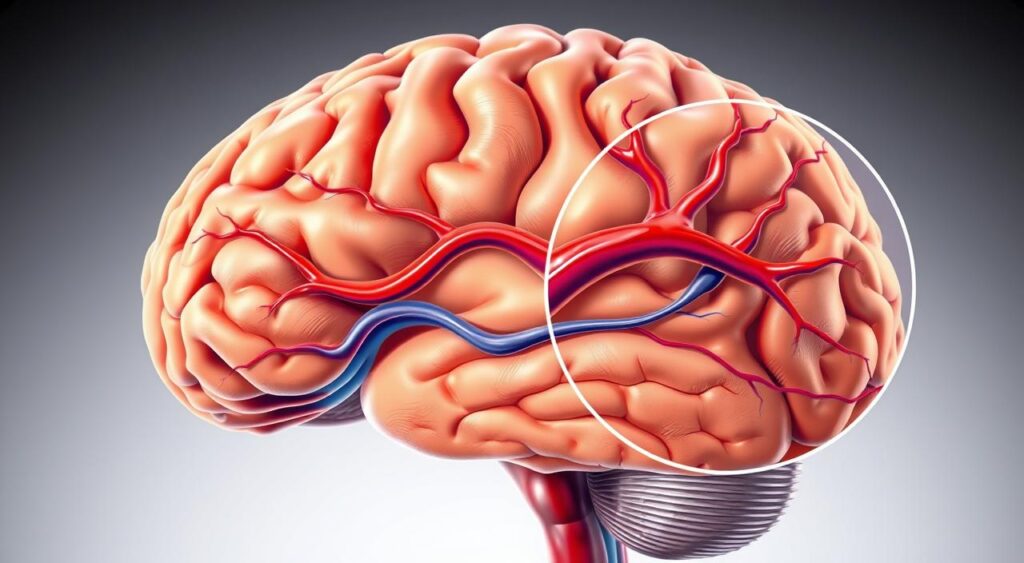
Anatomical Considerations
The brain’s venous system is a network of veins. It drains blood from the brain. The veins are divided into deep and superficial veins. Knowing the brain’s venous system is key to diagnosing and treating venous thrombosis.
The Impact of Brain Vein Thrombosis on Health
Intracranial venous thrombosis can greatly affect health, especially when blood clots in brain veins happen. This condition can cause symptoms like seizures, headaches, and vision changes. It also raises the risk of stroke and other serious issues.
Some common effects of brain vein thrombosis on health include:
- Neurological deficits, such as weakness or numbness in the face, arm, or leg
- Cognitive impairment, including memory loss and difficulty with concentration
- Emotional changes, such as depression and anxiety
It’s crucial to get medical help right away if symptoms of brain vein thrombosis show up. Quick treatment can lessen long-term damage and improve health outcomes. Managing blood clots in brain veins is key to avoiding more problems.
In severe cases, brain vein thrombosis can cause serious and even life-threatening issues. These may include:
- Stroke or cerebral hemorrhage
- Seizures or status epilepticus
- Hydrocephalus or increased intracranial pressure
Knowing the risks and effects of brain vein thrombosis is vital for those at risk. Recognizing blood clots in brain vein symptoms early can help get medical help fast. This can reduce the chance of lasting damage.
| Complication | Description |
|---|---|
| Stroke | A condition in which the brain does not receive enough oxygen and nutrients, leading to tissue damage |
| Seizures | Abnormal electrical activity in the brain, which can cause changes in behavior, sensation, or movement |
| Hydrocephalus | A condition in which fluid accumulates in the brain, leading to increased intracranial pressure |
Common Risk Factors and Causes
Brain vein thrombosis is a complex condition with many triggers. Knowing these risk factors is key for prevention and early detection. Genetic predisposition is a big factor, as some genes can raise the risk of brain blood clots.
Medical conditions like blood disorders, cancer, and autoimmune diseases also play a role. such as smoking, obesity, and using oral contraceptives can increase the risk too.
- Genetic predisposition
- Medical conditions, such as blood disorders and cancer
- Lifestyle factors, such as smoking and obesity
- Pregnancy and the postpartum period
Knowing these risk factors is crucial. Taking preventive steps can help lower the risk of brain vein thrombosis. By understanding the causes and risk factors, people can protect their health and prevent this serious condition.
| Risk Factor | Description |
|---|---|
| Genetic Predisposition | Certain genetic conditions can increase the risk of developing blood clots in the brain |
| Medical Conditions | Blood disorders, cancer, and autoimmune diseases can contribute to the development of brain vein thrombosis |
| Lifestyle Factors | Smoking, obesity, and oral contraceptive use can increase the risk of brain vein thrombosis |
Recognizing the Warning Signs
It’s key to spot cerebral venous thrombosis early for the best treatment. Symptoms include severe headaches, seizures, vision issues, and neurological problems. If you notice these signs, get medical help right away.
The symptoms of cerebral venous thrombosis depend on where and how big the clot is. Severe headaches are a common sign, feeling sudden and very intense. Other signs might be seizures, vision problems, and neurological deficits like weakness or numbness.
Some cases of cerebral venous thrombosis can be hard to diagnose because the symptoms are not clear. But knowing the warning signs helps you get medical help fast. This can lower the risk of serious problems and improve treatment results.
To spot the warning signs of cerebral venous thrombosis, remember these:
- Severe and sudden headaches
- Seizures or convulsions
- Vision problems, such as double vision or loss of vision
- Neurological deficits, such as weakness, numbness, or paralysis
Spotting these warning signs and getting medical help fast can greatly improve treatment for cerebral venous thrombosis. Knowing the symptoms and acting quickly can help avoid serious issues. This can also improve your life quality.
Diagnostic Approaches and Testing Methods
Diagnosing intracranial venous thrombosis, or cvt, involves several steps. These include imaging, lab tests, and clinical checks. The aim is to find out if there’s a blood clot in the brain’s veins and what caused it.
Imaging is key in finding cvt. Computed tomography (CT) scans, magnetic resonance imaging (MRI), and venography are used. They show where the clot is and if it’s harming the brain.
Imaging Techniques
- CT scans: provide detailed images of the brain’s venous system
- MRI: offers high-resolution images of the brain and its blood vessels
- Venography: involves injecting a contrast agent into the blood vessels to visualize the venous system
Lab tests also play a part. They help find out why cvt happened. This includes blood tests and genetic checks.
Laboratory Tests
Doctors also use clinical checks to diagnose cvt. They do a neurological exam and look at the patient’s health history. This helps spot risk factors and symptoms.
Treatment Strategies and Management
Treatment for intracranial blood clots often includes anticoagulation therapy. This helps dissolve clots and stops new ones from forming. In serious cases, thrombolytic drugs might be used to quickly break down the clot. Sometimes, surgery is needed too.
Managing symptoms and complications is key. This includes pain management, controlling seizures, and lowering intracranial pressure. Long-term care and follow-ups are also vital. They help prevent more problems and aim for the best recovery.
- Anticoagulation therapy: to prevent new clots from forming and to dissolve existing ones
- Thrombolytic drugs: to quickly dissolve the clot in severe cases
- Surgical interventions: may be necessary in certain situations
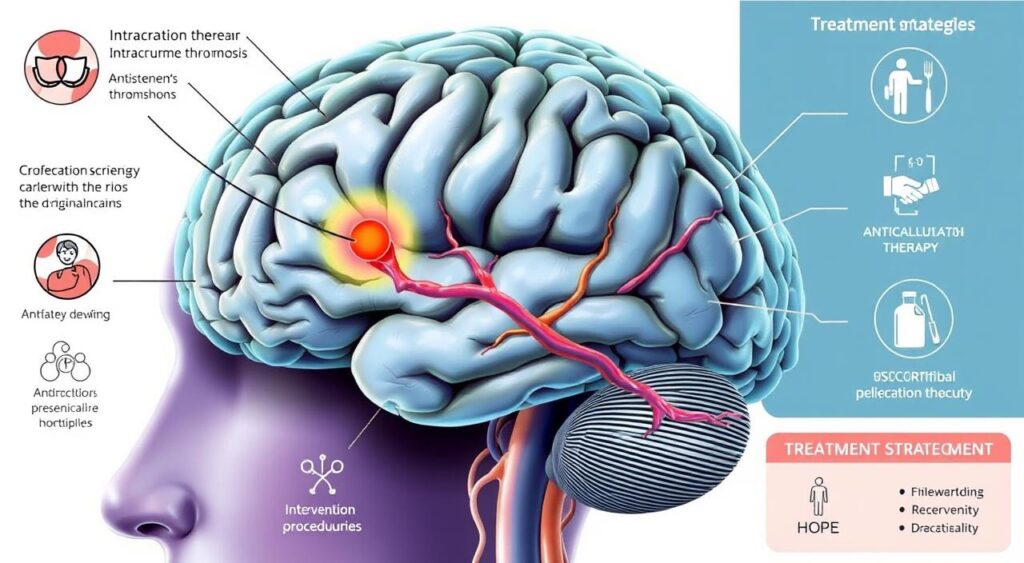
Knowing about treatment and management for intracranial blood clots helps patients. They can work with their doctors to create a good plan. This plan aims to manage their condition and lower the risk of more problems.
Complications and Long-term Prognosis
Having a brain vein clot can cause serious problems. Right away, you might see brain swelling, seizures, and a higher chance of stroke. These issues are urgent and need quick medical help.
Later on, you could face more issues like clotting again, lasting brain problems, and memory issues. A brain vein clot can really change your life. It can affect how you do everyday things, work, and connect with others. Finding ways to recover and adapt is key.
Immediate Complications
- Brain swelling
- Seizures
- Risk of stroke
Long-term Health Implications
Long-term, you might deal with clotting again and ongoing brain issues. Your thinking skills could also be affected, making it hard to remember, focus, or make decisions. It’s crucial to work with your healthcare team to manage these long-term effects.
Quality of Life Considerations
Dealing with a brain vein clot’s aftermath means thinking about your quality of life. You’ll need to adjust to any lasting effects, like brain or body problems, and find ways to stay independent. With the right support and therapy, you can learn to live with your condition and improve your life.
Prevention and Risk Reduction Measures
To prevent intracranial venous thrombosis, a mix of lifestyle changes and thrombosis treatment is needed. People with risk factors can lower their chances by drinking plenty of water, exercising, and not sitting still for too long. Those with certain health issues or family history might need to take medicine to prevent it.
Regular doctor visits are also crucial. They help catch and treat problems early, which can lower the risk of thrombosis. Taking these steps can greatly reduce the chance of getting intracranial venous thrombosis. Some ways to prevent it include:
- Staying physically active to improve blood flow and overall health
- Avoiding smoking and limiting alcohol consumption
- Maintaining a healthy weight to reduce pressure on veins
- Managing underlying medical conditions, such as high blood pressure or diabetes
By making these habits part of their daily routine, people can lower their risk of intracranial venous thrombosis and stay healthier.

| Preventive Measure | Description |
|---|---|
| Lifestyle Modifications | Staying hydrated, exercising regularly, and avoiding prolonged immobility |
| Anticoagulation Therapy | Preventive treatment for individuals with certain medical conditions or genetic predispositions |
| Regular Medical Check-ups | Early detection and prompt treatment of underlying conditions that may increase the risk of thrombosis |
Conclusion: Living with and Managing Intracranial Venous Thrombosis
Intracranial venous thrombosis (CVT) can be serious, but many people recover well. The key is to recognize the symptoms of CVT and get help right away. Knowing the risks, signs, and treatments helps people take charge of their health.
Research and new treatments are making a big difference. Patients and families should keep up with the latest news. This way, they can face the challenges of CVT together and live well.
FAQ
Q: What is intracranial venous thrombosis?
A: Intracranial venous thrombosis, or CVT, is a rare condition. It happens when blood clots form in the brain’s veins. These veins are located between the brain and the skull.
Q: What are the different types of cerebral venous thrombosis?
A: There are several types of cerebral venous thrombosis. These include cortical vein thrombosis, deep venous thrombosis, and sinus thrombosis. Each type is based on where and how much the blood clot forms in the brain’s veins.
Q: How does intracranial venous thrombosis affect brain health?
A: Blood clots in the brain’s veins can cause problems. They can lead to increased pressure in the brain. This may cause severe headaches, seizures, vision issues, and cognitive problems.
If not treated, it can lead to serious issues. These include brain damage and stroke.
Q: What are the common risk factors for brain vein thrombosis?
A: Several factors increase the risk of brain vein thrombosis. These include genetic conditions, certain medical issues, and pregnancy. Other risks include using oral contraceptives, smoking, and being immobile for a long time.
Q: What are the warning signs of cerebral venous thrombosis?
A: Warning signs include severe headaches, seizures, vision problems, and neurological issues. These symptoms depend on where and how big the blood clot is.
Q: How is intracranial venous thrombosis diagnosed?
A: Doctors use imaging like CT scans and MRI to diagnose it. They also do lab tests to find underlying conditions. A thorough clinical assessment is also done.
Q: What are the treatment options for intracranial blood clots?
A: The main treatment is anticoagulation therapy. It helps dissolve the clot and prevent new ones. In severe cases, thrombolytic drugs or surgery might be needed. Managing symptoms and long-term care are also key.
Q: What are the potential complications and long-term prognosis for individuals with brain vein clots?
A: Immediate risks include brain swelling, seizures, and stroke. Long-term, there’s a chance of recurring clots and lasting neurological problems. With quick treatment, many people recover well and live a good life.
Q: How can intracranial venous thrombosis be prevented?
A: Preventive steps include a healthy lifestyle and avoiding immobility. For those at risk, anticoagulation therapy might be recommended. Regular check-ups and treating underlying conditions help prevent brain vein clots.
