Osteoporosis is a silent epidemic that affects over 200 million people worldwide. It causes devastating bone loss and increases the risk of fractures. This disease is often overlooked, with one in three women and one in five men over 50 experiencing a fracture.
Understanding the types and facts about osteoporosis is key to managing bone health. It helps prevent life-altering consequences.

Key Takeaways
- Osteoporosis is a chronic condition that causes progressive bone density loss, increasing the risk of fractures.
- There are various types of osteoporosis, including age-related, secondary, and postmenopausal forms.
- Osteoporosis affects millions globally, with significant health and economic implications.
- Early detection and proactive management are essential for maintaining bone health and preventing debilitating fractures.
- Comprehensive understanding of osteoporosis diseases, their causes, and available treatments is crucial for effective prevention and management.
What is Osteoporosis and Its Impact on Bone Health
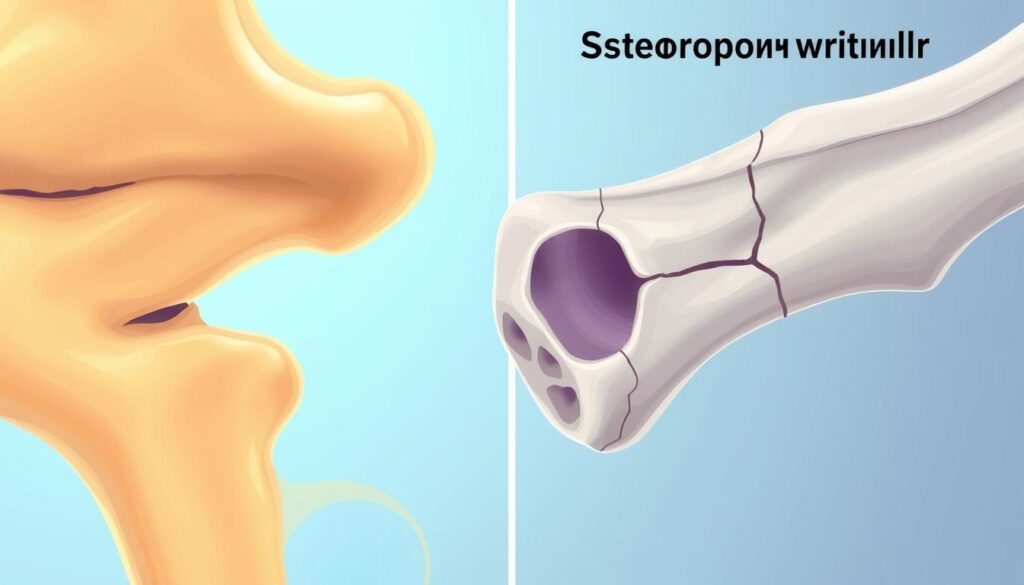
Osteoporosis is a common bone disease. It causes bones to lose density and mass over time. This makes bones weak and prone to breaking, making simple tasks hard.
It’s important to understand how osteoporosis affects bone health. This knowledge helps keep our bones strong and resilient.
Understanding Bone Mass and Density
Bones are living tissues that constantly renew and remodel themselves. Bone mass is the total amount of bone in our skeleton. Bone density measures the mineral content in a specific bone area.
Keeping bone mass and density at their best is key. It helps prevent bone density loss and keeps bones healthy.
The Progressive Nature of Bone Loss
As we age, our bones naturally lose mass and density. This is called bone loss. Factors like calcium deficiency and vitamin D deficiency can speed up this process.
This gradual loss can lead to osteoporosis if not managed. Osteoporosis increases the risk of fractures and other bone problems.
| Bone Health Indicators | Optimal Levels | Factors Contributing to Bone Loss |
|---|---|---|
| Bone Mineral Density (BMD) | T-score above -1.0 | Aging, Hormonal Changes, Sedentary Lifestyle, Malabsorption Disorders |
| Calcium Intake | 1,000-1,200 mg per day | Calcium Deficiency, Inadequate Dietary Intake, Malabsorption |
| Vitamin D Levels | 30-80 ng/mL | Vitamin D Deficiency, Insufficient Sun Exposure, Liver or Kidney Disorders |
“Osteoporosis is a silent disease, meaning it can progress without any obvious symptoms until a fracture occurs.”
Common Types of Osteoporosis Diseases
Osteoporosis comes in many forms, each with its own set of characteristics. Knowing about these types is key to fighting this widespread problem.
Postmenopausal osteoporosis mainly hits women after menopause. It’s linked to hormonal changes, causing a drop in estrogen and bone loss.
Senile osteoporosis is tied to aging and affects older adults of both genders. As we age, keeping bones strong gets harder, raising the risk of fractures.
Secondary osteoporosis is caused by other health issues or certain meds. Things like hormonal imbalances, chronic diseases, and some cancer treatments can lead to it, increasing fracture risk.
| Type of Osteoporosis | Characteristics | Contributing Factors |
|---|---|---|
| Postmenopausal Osteoporosis | Primarily affects women after menopause | Hormonal changes, decline in estrogen levels |
| Senile Osteoporosis | Associated with the natural aging process | Decreased ability to maintain bone health with age |
| Secondary Osteoporosis | Develops due to underlying medical conditions or medication use | Hormonal imbalances, chronic inflammation, cancer treatments |
Understanding osteoporosis types and their causes helps in creating better prevention and treatment plans. This can help reduce fracture risks.
Primary vs. Secondary Osteoporosis: Key Differences
Osteoporosis is a serious bone disease with two main types: primary and secondary. Knowing the differences between them is key for managing and treating the disease.
Age-Related Osteoporosis
Primary osteoporosis is the most common type. It’s linked to aging. As we age, our bones lose mass, making them weaker and more prone to fractures.
This type is especially common in postmenopausal women. Hormonal changes speed up bone loss in them.
Medical Condition-Induced Osteoporosis
Secondary osteoporosis is caused by medical conditions or medications. Issues like hormonal imbalances, chronic diseases, and nutritional deficiencies can lead to it. Patients with this type need treatments that target the root causes.
It’s important for doctors to know the difference between primary and secondary osteoporosis. This helps them create better prevention and treatment plans. By focusing on the specific risk factors and hormonal changes or medical conditions, patients can protect their bones and avoid serious fractures.
Early Warning Signs and Symptoms
Osteoporosis is a silent disease that often goes unnoticed in its early stages. However, there are early signs that can signal its onset. Knowing these signs is key to getting diagnosed early and treating it effectively. This can help prevent fracture risk and bone density loss.
One early sign is losing height over time. As bones weaken, the spine curves, leading to a noticeable height drop. This height loss often comes with back pain, ranging from mild to severe.
Another sign is being more prone to fractures from minor injuries or falls. Osteoporosis can cause fractures in the wrists, hips, and spine, even with little trauma.
Lastly, calcium deficiency can also lead to osteoporosis. Symptoms like muscle cramps, tingling, or numbness can indicate low calcium levels and bone loss.
- Gradual height loss
- Persistent back pain
- Increased risk of fractures
- Muscle cramps and tingling sensations
It’s vital to catch osteoporosis early to manage it effectively. If you notice these signs, see a healthcare professional for a thorough check-up and treatment plan.
| Symptom | Description | Relationship to Osteoporosis |
|---|---|---|
| Height Loss | Gradual decrease in overall stature | Weakening of the bones, leading to spinal curvature and compression |
| Back Pain | Persistent or worsening discomfort in the back | Spinal fractures and vertebral deformities associated with bone loss |
| Fractures | Increased susceptibility to breaks, even from minor injuries | Decreased bone density and strength, making bones more prone to fractures |
| Calcium Deficiency | Muscle cramps, tingling sensations, and numbness | Imbalance in calcium levels, contributing to the development of osteoporosis |
Risk Factors Contributing to Bone Density Loss
Osteoporosis is a complex condition influenced by various risk factors. Understanding these factors is crucial for effective prevention and management. Let’s explore the key contributors to bone density loss.
Genetic Predisposition
Family history plays a significant role in an individual’s risk of developing osteoporosis. Certain genetic variations can make people more susceptible to reduced bone mass and increased fragility. Individuals with a close relative who has been diagnosed with osteoporosis are more likely to experience the condition themselves.
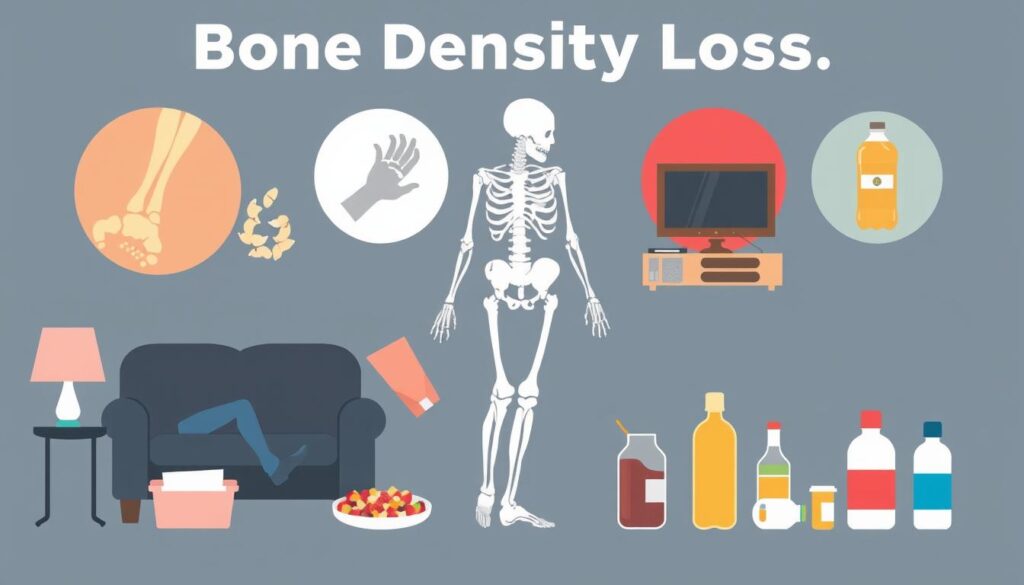
Lifestyle-Related Factors
Lifestyle choices can have a profound impact on bone health. Factors such as insufficient calcium and vitamin D intake, lack of weight-bearing exercise, smoking, and excessive alcohol consumption can all contribute to the gradual loss of bone density over time.
- Poor dietary habits, including low intake of calcium and vitamin D, can lead to calcium deficiency and impaired bone mineralization.
- Sedentary lifestyle and lack of weight-bearing physical activity can hinder the development and maintenance of strong bones.
- Smoking and excessive alcohol use can disrupt the delicate balance of bone formation and resorption, accelerating bone loss.
Medical Conditions
Certain medical conditions can also increase the risk of osteoporosis. These include endocrine disorders (such as thyroid or parathyroid dysfunction), inflammatory conditions (like rheumatoid arthritis), and gastrointestinal diseases (including celiac disease and inflammatory bowel disease) that can interfere with nutrient absorption.
| Risk Factor | Description |
|---|---|
| Genetic Predisposition | Family history and genetic variations that increase susceptibility to osteoporosis. |
| Lifestyle-Related Factors | Insufficient calcium and vitamin D intake, lack of weight-bearing exercise, smoking, and excessive alcohol consumption. |
| Medical Conditions | Endocrine disorders, inflammatory conditions, and gastrointestinal diseases that can impact bone health. |
“Understanding the risk factors for osteoporosis is the first step in developing an effective prevention and management plan.”
The Role of Calcium and Vitamin D in Bone Health
Keeping bones strong is key for good health. Calcium and vitamin D are two important nutrients for this. They help prevent calcium deficiency and vitamin D deficiency, which can cause osteoporosis and other bone problems.
Calcium is found mainly in bones and teeth. It’s essential for building and keeping bones dense. Adults need 1,000-1,200 mg of calcium each day. Good sources include dairy, leafy greens, fortified foods, and some fish.
Vitamin D helps our body use calcium. Without enough vitamin D, we can’t use the calcium we eat. Adults should get 600-800 IU of vitamin D daily. Good sources are sunlight, fatty fish, and foods fortified with vitamin D.
It’s important to prevent calcium deficiency and vitamin D deficiency to keep bones healthy. Regular health checks, supplements if needed, and a diet full of these nutrients can help. This can lower the risk of osteoporosis and other bone issues.
“Calcium and vitamin D work together to build and maintain strong bones. It’s important to get enough of both for optimal bone health.”
Hormonal Changes and Their Effect on Bone Density
Hormonal changes are key to keeping our bones healthy. Osteoporosis, a condition where bones lose density, often comes from hormonal imbalances. This is especially true for women going through menopause and men with declining testosterone levels.
Menopause and Osteoporosis
As women near menopause, their ovaries make less estrogen. Estrogen is vital for strong bones. Without enough estrogen, women lose bone density fast, making them more likely to get osteoporosis.
During menopause, the body’s hormonal changes cause a quick loss of bone mass. This increases the risk of fractures and other problems.
Testosterone Levels and Male Bone Health
Osteoporosis isn’t just a women’s issue; it affects men too. As men age, their testosterone levels drop. This can cause bone density loss and raise the risk of osteoporosis.
It’s important for doctors to understand how hormonal changes affect bone health in men. This helps them provide better care for men’s bone health, especially as they get older.
Dealing with the hormonal changes that lead to osteoporosis is key. Healthcare professionals need to know the risk factors for both women and men. This way, they can offer tailored care to keep bones strong.

Diagnostic Methods and Screening Tests
Early detection is key in managing bone density loss and lowering fracture risk. Doctors use different tests to check bone health and spot osteoporosis early. The dual-energy X-ray absorptiometry (DXA) scan is a top choice. It measures bone mineral density (BMD) very accurately.
DXA scans are the best way to find osteoporosis. They look at bone density in key areas like the spine, hip, and wrist. These areas are more likely to break. The scans also show how bone density changes over time. This helps doctors see how well treatments are working.
Other imaging methods, like quantitative computed tomography (QCT) and peripheral QCT (pQCT), are also used. They give more detailed info about bone quality and structure. This helps in early detection and managing osteoporosis.
Regular checks are vital for keeping bones healthy. Early action can greatly improve outcomes and lower the chance of serious fractures. Doctors might suggest regular bone density tests for people at higher risk, like postmenopausal women or those with certain health issues.
“Osteoporosis is a silent disease, and the first sign is often a fracture. That’s why it’s so important to get regular bone density tests and take proactive steps to maintain bone health.”
Knowing about different tests and getting regular screenings helps people manage their bone health. This can lessen the effects of osteoporosis.
Prevention Strategies for Maintaining Bone Health
Keeping your bones strong is key. By using the right prevention strategies, you can keep your bones healthy. This includes regular exercise and a diet that supports bone health. These steps can help fight osteoporosis and lower the chance of fractures.
Exercise and Physical Activity
Exercise is vital for bone health. Activities like walking, jogging, and dancing help build strong bones. They stimulate cells that make bones. Also, exercises that make muscles stronger can improve bone density.
- Aim for at least 30 minutes of weight-bearing exercise most days of the week.
- Incorporate strength-training exercises, such as weightlifting or resistance band workouts, at least two to three times a week.
- Consider low-impact activities like swimming or cycling to complement your weight-bearing exercises.
Nutritional Guidelines
Eating a balanced diet rich in calcium is crucial. Make sure you get enough calcium, vitamin D, and other nutrients. These help build and strengthen bones.
- Incorporate calcium-rich foods, such as dairy products, leafy greens, and fortified cereals, into your daily meals.
- Supplement with vitamin D, which aids in the absorption of calcium, especially if your exposure to sunlight is limited.
- Limit your intake of sodium, protein, and caffeine, as they can contribute to calcium deficiency and bone loss.

By following these prevention strategies, you can protect your bone health. Making lifestyle changes that support strong bones can help you stay independent. It lets you live a vibrant, active life.
Modern Treatment Options and Medications
Managing osteoporosis now involves a wide range of treatments. These options help lower the risk of fractures and boost bone density. They aim to tackle the root causes of bone loss, helping patients keep their bones strong.
Bisphosphonates: Preserving Bone Density
Bisphosphonates are a type of medicine that stops bone breakdown. They are very effective in slowing down bone density loss and cutting down fracture risk. Alendronate, risedronate, and zoledronic acid are some common bisphosphonates that have shown great results in studies.
Hormone Therapy: Restoring Balance
Hormone therapy is a good choice for postmenopausal women with osteoporosis. It helps keep bone mass and stops bone density loss. Selective estrogen receptor modulators (SERMs) are another hormone-based treatment that helps with bone health.
Newer Biological Agents: Targeted Approaches
New biological agents like denosumab and teriparatide have been developed. They target specific cells to stop bone loss or make new bone. This offers new ways to lower fracture risk and strengthen bones.
| Treatment Option | Mechanism of Action | Key Benefits |
|---|---|---|
| Bisphosphonates | Inhibits bone resorption | Slows bone density loss, reduces fracture risk |
| Hormone Therapy | Restores hormonal balance | Maintains bone mass, prevents further bone density loss |
| Biological Agents | Targeted inhibition or stimulation of bone cells | Addresses fracture risk, improves overall bone strength |
Choosing the right treatment option for osteoporosis is a team effort. It involves the patient and their doctor, considering factors like age, medical history, and how severe the condition is. With these modern treatments, people with osteoporosis can protect their bones and lower the chance of serious fractures.
Lifestyle Modifications for Managing Osteoporosis
Keeping your bones strong is key when you have osteoporosis. Medications and treatments are important, but lifestyle changes can help too. Here are some simple steps to boost your bone health and improve your life.
Daily Activities and Safety Measures
Doing regular physical activities is great for your bones and preventing falls. Try walking, jogging, or dancing for 30 minutes each day. Also, add balance and flexibility exercises to get better at staying steady and moving.
- Choose low-impact exercises like swimming or cycling to be gentle on your joints.
- Stay away from activities that involve sudden or high-impact moves to lower fracture risk.
- Get a custom exercise plan from your doctor that fits your fitness level and health.
Home Environment Modifications
Changing your home can also help prevent falls and fractures. Take a close look at your living space and make changes to make it safer and easier to move around.
- Put handrails on both sides of stairs and grab bars in bathrooms for extra support.
- Make sure your home is well-lit, especially in busy areas and on stairs.
- Get rid of tripping hazards by securing rugs, cords, and clutter, and replace slippery floors with safer ones.
- Adjust the height of furniture, like chairs and beds, to make sitting and standing easier.
By making these lifestyle changes, you can actively manage your osteoporosis. This helps you stay independent and lowers the chance of serious fractures. A mix of medical care, exercise, and a safe home is key to good bone health and a better life.
The Connection Between Diet and Bone Strength
Keeping our bones strong is key at every age. Our diet is a big part of this. Certain nutrients are especially important for bone health.
Calcium is a top nutrient for bones. It’s the main mineral in bones. Not enough calcium can lead to calcium deficiency and osteoporosis. Eating dairy, leafy greens, nuts, and fortified foods helps meet calcium needs.
Vitamin D is also crucial. It helps our body use calcium. A vitamin D deficiency can raise the risk of osteoporosis. Good sources include sunlight, fatty fish, and fortified foods.
- Eat foods high in calcium like dairy, leafy greens, and fortified foods.
- Get enough vitamin D from sunlight, fatty fish, and supplements if needed.
- Follow a balanced diet to keep bones strong and avoid calcium deficiency and vitamin D deficiency.
Eating right can help strengthen your bones and lower osteoporosis risk. Focus on a diet full of nutrients to keep bones healthy for life.
Exercise Programs and Physical Therapy Approaches
Keeping active is key for those with osteoporosis. It helps prevent further bone density loss and lowers fracture risk. Targeted exercise and physical therapy guidance are very helpful.
Walking, jogging, or dancing are great for strengthening bones. Resistance training with weights or bands boosts bone and muscle strength. This is vital for lowering fall risk.
- Swimming or cycling are good for heart health without harming bones.
- Tai Chi or yoga improve balance and coordination, reducing falls.
Physical therapists are essential in creating exercise plans for osteoporosis patients. They assess needs, devise a comprehensive exercise plan, and teach proper technique for safe workouts.
| Exercise Type | Benefits |
|---|---|
| Weight-bearing exercises | Stimulate bone growth, improve strength and balance |
| Resistance training | Increase muscle strength and bone density |
| Balance exercises | Improve stability and coordination, reduce fall risk |
By adopting prevention strategies and lifestyle modifications, people with osteoporosis can manage their bone density and health.
Living with Osteoporosis: Daily Management Tips
Living with osteoporosis can be tough, but there are ways to manage it. You can keep your bones healthy and live an active life. This section will give you tips on pain management and finding emotional support.
Pain Management Strategies
Pain from osteoporosis is a big issue. But, there are ways to ease it. For mild pain, try over-the-counter meds like acetaminophen or NSAIDs. For more pain, your doctor might prescribe stronger meds or creams.
Also, try heat or cold therapy, massage, and gentle exercises. These can help a lot with pain.
Emotional Support and Resources
Osteoporosis can affect your mood. Joining support groups, online or in-person, can help. You’ll find people who understand you and get advice.
Healthcare providers can also connect you with mental health experts. These resources can help you stay positive and manage the condition better.
| Lifestyle Modifications | Treatment Options | Prevention Strategies |
|---|---|---|
| Incorporating regular exercise Maintaining a balanced, calcium-rich diet Avoiding high-risk activities Ensuring a safe home environment | Prescription medications Physical therapy and rehabilitation Complementary therapies (e.g., acupuncture, massage) Pain management techniques | Regular bone density screenings Consuming adequate calcium and vitamin D Engaging in weight-bearing exercises Maintaining a healthy lifestyle |
By using lifestyle changes, treatments, and prevention, you can manage osteoporosis. This way, you can improve your life quality.
Remember, every person’s osteoporosis journey is different. It’s key to work with your healthcare team to create a plan that’s right for you.
Conclusion
In this detailed article, we’ve looked into osteoporosis diseases. We’ve covered their types, causes, and how they affect bone health. We’ve also talked about bone mass, density, and the differences between primary and secondary osteoporosis.
Now, readers know how to protect their bones. We’ve talked about the importance of calcium, vitamin D, and hormones. This helps keep bones strong. We’ve also discussed how to spot early signs and risk factors.
This article is a complete guide to osteoporosis diseases. It covers prevention strategies and treatment options. It gives readers the tools to make smart choices for their bone health and overall well-being.
FAQ
Q: What is osteoporosis and how does it impact bone health?
A: Osteoporosis is a condition where bones lose mass and density. This makes bones weak and more likely to break. It affects the skeletal system, increasing the risk of fractures in hips, spine, and wrists.
Q: What are the different types of osteoporosis diseases?
A: There are several types of osteoporosis. Postmenopausal osteoporosis happens due to hormonal changes in women. Senile osteoporosis is age-related. Secondary osteoporosis is caused by medical conditions or medications.
Q: What are the risk factors for developing osteoporosis?
A: Several factors increase the risk of osteoporosis. These include genetics, age, gender, hormonal changes, and diet. A sedentary lifestyle and certain medical conditions also play a role.
Q: How can calcium and vitamin D support bone health?
A: Calcium and vitamin D are key for strong bones. Calcium is the main mineral in bones, and vitamin D helps the body use calcium. Getting enough of these through diet or supplements is vital.
Q: What are the early warning signs and symptoms of osteoporosis?
A: Early signs of osteoporosis include losing height, back pain, and a stooped posture. You may also find you break bones more easily. These symptoms develop slowly as bone density drops.
Q: How are osteoporosis and hormonal changes related?
A: Hormonal changes, like the drop in estrogen in women or testosterone in men, can lead to osteoporosis. These changes affect bone remodeling, causing bone loss.
Q: What diagnostic methods are used to detect osteoporosis?
A: The DXA scan is the main tool for diagnosing osteoporosis. It measures bone density and gives a T-score. Other tests may include bone turnover markers and imaging to check bone structure and fracture risk.
Q: What are the modern treatment options for osteoporosis?
A: Modern treatments include medications like bisphosphonates and hormone therapy. Biological agents also help improve bone density. Lifestyle changes, such as exercise and diet, are also part of treatment.
Q: How can lifestyle changes help manage osteoporosis?
A: Lifestyle changes are key in managing osteoporosis. Regular exercise, balance training, and muscle-strengthening activities help. Eating foods rich in calcium and vitamin D and making your home safer also helps.
