Did you know that nearly 1 in 4 women worldwide face menstrual disorders? These can range from delayed periods to no periods at all. Such issues can greatly affect a woman’s health and happiness. This guide will cover the reasons, signs, and ways to treat menstrual delays and related problems.
It aims to help women dealing with irregular periods. It also offers expert advice on managing these issues.
Key Takeaways
- Menstrual disorders, such as delayed or absent periods, can have a significant impact on a woman’s reproductive health.
- Understanding the normal menstrual cycle and its variations is crucial for identifying and addressing menstrual irregularities.
- Common causes of menstrual postponement include hormonal imbalances, genetic factors, and underlying health conditions like PCOS and thyroid dysfunction.
- Seeking professional medical advice is essential for diagnosing and effectively managing menstrual disorders.
- Incorporating lifestyle changes, stress management techniques, and natural remedies can complement medical treatment for improved menstrual health.
Understanding Menstrual Cycle Basics and Normal Patterns
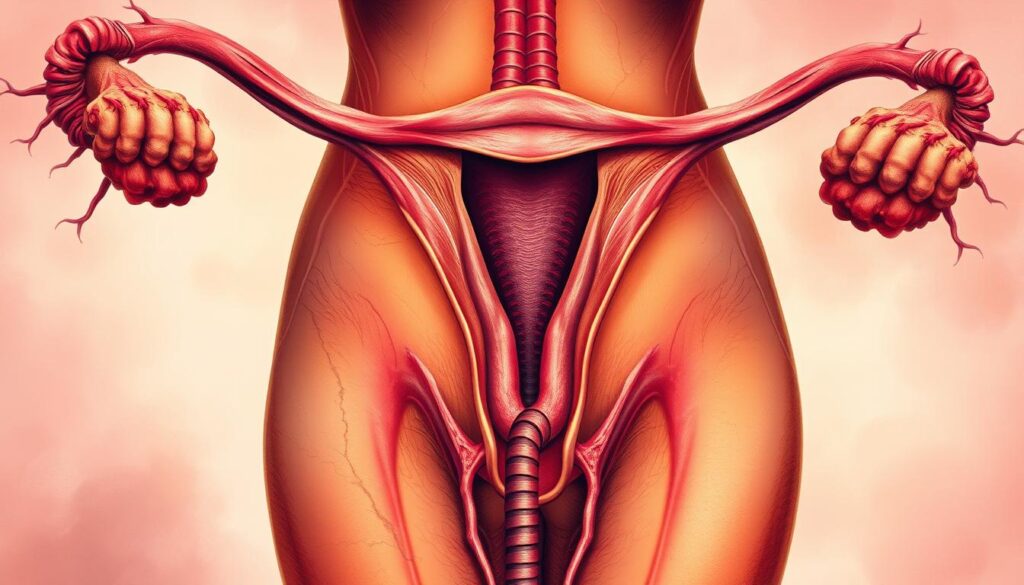
The menstrual cycle is key to a woman’s health. It has four main phases, each with its own set of hormones. These phases are important for a woman’s body to work right.
The Four Phases of Menstrual Cycle
- Menstrual Phase: This is when the uterine lining sheds, causing bleeding. It’s often called a period.
- Follicular Phase: Here, the ovaries get ready to release an egg. The uterine lining also gets thicker, ready for a fertilized egg.
- Ovulation Phase: This is when the egg is released from the ovary. It’s the main event of this phase.
- Luteal Phase: After ovulation, the leftover follicle turns into the corpus luteum. It makes hormones to get the uterine lining ready for an egg.
Normal Menstrual Cycle Length and Variations
The usual cycle lasts from 21 to 35 days, with 28 days being average. But, cycles can vary. Age, stress, and health can change how long and regular a cycle is.
Hormones Controlling Menstruation
Hormones like estrogen, progesterone, FSH, and LH control the cycle. They work together to start each phase. This ensures the reproductive system works well.
“The menstrual cycle is a remarkable, intricate process that showcases the delicate balance of the female reproductive system.”
Knowing about the menstrual cycle and its hormones is vital. It helps keep reproductive health in check. It also helps spot any issues or irregularities.
Common Causes of Postponement of Menstruation Diseases
Menstrual cycle problems, like amenorrhea (no menstruation) and oligomenorrhea (menstruation that’s too infrequent), have many causes. Knowing what leads to postponement of menstruation is key to tackling these health issues.
Hormonal imbalances are a big reason for menstrual delays. Issues like polycystic ovary syndrome (PCOS), thyroid problems, and birth control can upset hormone levels. This can cause amenorrhea or oligomenorrhea.
Stress, whether physical or emotional, can also mess with your cycle. Long-term stress can upset the body’s hormonal balance. This is tough for people with stressful lives or big life changes.
Some medical issues, like eating disorders, can also delay menstruation. Conditions like anorexia nervosa and bulimia nervosa can lead to weight loss and hormone problems. This often results in amenorrhea.
| Cause | Description |
|---|---|
| Hormonal Imbalances | Conditions like PCOS, thyroid dysfunction, and hormonal contraceptive use can disrupt the balance of reproductive hormones, leading to menstrual cycle delays. |
| Stress | Chronic physical and emotional stress can interfere with the hypothalamic-pituitary-ovarian axis, resulting in amenorrhea or oligomenorrhea. |
| Medical Conditions | Eating disorders, such as anorexia nervosa and bulimia nervosa, can cause significant weight loss and hormonal imbalances, leading to amenorrhea. |
Knowing the common reasons for menstrual delays is the first step to fixing these health issues. Getting medical help and making lifestyle changes can help get your cycle back on track. This supports your reproductive health.
Primary Amenorrhea: Causes, Symptoms, and Risk Factors
Primary amenorrhea is when someone hasn’t had their first period. It’s a complex issue with many causes. These include genetic and anatomical problems, and hormonal imbalances.
Genetic and Anatomical Factors
Genetic disorders like Turner syndrome can cause primary amenorrhea. They affect the reproductive organs’ development. Anatomical issues, such as uterine abnormalities or blockages, also delay menstruation.
Hormonal Imbalances Leading to Primary Amenorrhea
Hormonal imbalances, especially in estrogen, progesterone, and gonadotropins, affect menstruation. Conditions like PCOS or dysfunction in the hormonal axis can disrupt this balance. This leads to delayed menstruation.
Diagnostic Approaches
Diagnosing primary amenorrhea involves a detailed evaluation. This includes a medical history, physical exam, and specialized tests. Blood tests check hormone levels, imaging studies look at the reproductive organs, and genetic testing may be done.
| Common Causes of Primary Amenorrhea | Symptoms | Risk Factors |
|---|---|---|
| Genetic disorders (e.g., Turner syndrome) Anatomical abnormalities (e.g., uterine malformations) Hormonal imbalances (e.g., PCOS, hypothalamic dysfunction) | Delayed or absent onset of menstruation Lack of secondary sexual characteristics Infertility or difficulty conceiving | Family history of genetic conditions Underlying medical conditions (e.g., thyroid disorders) Extreme physical or emotional stress |
Understanding primary amenorrhea’s causes, symptoms, and risk factors helps healthcare providers. They can then create tailored treatment plans. This aims to help individuals achieve their reproductive health goals.
Secondary Amenorrhea and Its Impact on Reproductive Health
Menstrual disorders can greatly affect a woman’s reproductive health. Secondary amenorrhea is a condition that needs attention. It’s when a woman stops getting her period for at least three months, even if she used to get it regularly.
The reasons for secondary amenorrhea vary. They can include hormonal imbalances, medical conditions, stress, or changes in weight. Knowing the cause is key to finding the right treatment.
Secondary amenorrhea can upset the balance of the reproductive system. It can cause low bone density, heart disease risks, and infertility. Also, conditions like polycystic ovary syndrome or thyroid problems might need specific treatments.
“Addressing secondary amenorrhea is not just about restoring regular menstrual cycles; it’s about safeguarding a woman’s overall reproductive health and wellbeing.”
It’s important to keep an eye on secondary amenorrhea and seek medical help quickly. Working with doctors, women can tackle the causes and protect their reproductive health and menstrual disorders.

Polycystic Ovary Syndrome (PCOS) and Menstrual Irregularities
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder that affects many women of reproductive age. It causes menstrual irregularities, which can greatly affect a woman’s reproductive health.
PCOS Symptoms and Diagnosis
PCOS symptoms include irregular or absent periods, too much facial and body hair, acne, and weight issues. Doctors diagnose PCOS by looking at medical history, doing physical exams, and running tests like blood work and ultrasound.
Treatment Options for PCOS-Related Menstrual Issues
There are many treatments for PCOS-related menstrual issues. These include:
- Hormonal birth control pills to regulate the menstrual cycle
- Metformin, an insulin-sensitizing medication, to improve ovulation and regulate menstrual cycles
- Anti-androgen medications to reduce the effects of excess male hormones
- Ovulation-inducing medications to stimulate regular ovulation
Lifestyle Modifications for PCOS Management
Lifestyle changes are also key in managing PCOS. These include:
- Eating a balanced, low-glycemic diet to regulate insulin levels
- Regular exercise to maintain a healthy weight and improve insulin sensitivity
- Stress management techniques, such as yoga or meditation, to reduce the impact of stress on hormone imbalances
- Quitting smoking, as it can worsen PCOS symptoms
By addressing the causes of PCOS and using a comprehensive treatment plan, women can better control their menstrual cycles and reproductive health.
| PCOS Symptom | Prevalence |
|---|---|
| Irregular menstrual periods | 70-90% |
| Excess facial/body hair growth | 60-70% |
| Acne | 50-70% |
| Difficulty with weight management | 80-90% |
“With the right treatment and lifestyle changes, women with PCOS can take control of their menstrual health and improve their overall quality of life.”
Thyroid Dysfunction and Its Effect on Menstrual Cycles
Hormones play a key role in keeping menstrual cycles regular. When thyroid disorders disrupt this balance, it can harm women’s reproductive health.
Hypothyroidism and hyperthyroidism can greatly affect menstrual cycles. Thyroid dysfunction can cause irregularities like delayed or missing periods.
In hypothyroidism, thyroid hormone shortage can make periods longer and more irregular. It might even stop menstruation. On the other hand, hyperthyroidism can make periods shorter and lighter.
Thyroid disorders can also lead to infertility, miscarriage, and PCOS. These issues are due to hormonal imbalances caused by thyroid problems.
“Thyroid disorders can have a significant impact on the menstrual cycle, often leading to irregular, delayed, or even absent periods. Addressing the underlying thyroid dysfunction is crucial for restoring hormonal balance and regular menstrual patterns.”
Fixing thyroid-related menstrual issues often requires a full plan. This includes medication, lifestyle changes, and sometimes special treatments for reproductive health.
Knowing how thyroid dysfunction affects menstrual cycles helps women manage their reproductive health. They can work towards regular and healthy periods.
Stress-Related Menstrual Disorders: Understanding the Mind-Body Connection
The link between stress and menstrual health is getting more attention. Psychological factors can really affect how regular and severe menstrual cycles are. It’s key to understand this connection to manage menstrual issues well.
Psychological Factors Affecting Menstruation
Stress, anxiety, and depression can mess with the hormonal balance needed for a normal menstrual cycle. Chronic stress can mess with hormone production and regulation. This can lead to late or missed periods and more severe premenstrual symptoms.
Emotional trauma, big life events, and daily stress can all cause menstrual problems. The body’s stress response can disrupt the reproductive system. This leads to changes that show up as menstrual irregularities.
Stress Management Techniques
- Practicing mindfulness and meditation to reduce stress and promote relaxation
- Engaging in regular exercise, such as yoga or tai chi, to manage stress and improve overall well-being
- Prioritizing self-care activities, like getting enough sleep, maintaining a healthy diet, and finding time for hobbies
- Seeking support from a mental health professional, such as a therapist or counselor, to address underlying psychological factors
Using effective stress management can help reduce the impact of psychological factors on menstrual health. Tackling the mind-body connection is vital for managing menstrual disorders and improving reproductive health.
“The mind and body are not separate, but rather, they are intimately connected. Addressing the psychological and emotional aspects of menstrual disorders can have a profound impact on physical health.”
Endometriosis and Its Role in Menstrual Disorders
Endometriosis is a chronic condition that affects 176 million women worldwide. It happens when tissue from the uterus grows outside the uterus. This tissue can grow on organs like the ovaries, fallopian tubes, bladder, or intestines.
This misplaced tissue acts like the uterine lining. It thickens, breaks down, and bleeds with each menstrual cycle. This leads to various symptoms.
One main symptom is pelvic pain, which can be very severe. Women with endometriosis often have painful menstrual cramps and heavy or irregular periods. They may also struggle with infertility.
The location and extent of the endometrial implants can cause other symptoms. These include pain during sex, bowel movements, or urination.
Diagnosing endometriosis can be hard because symptoms vary and can look like other conditions. Doctors use medical history, physical exams, and imaging tests like ultrasound or MRI. Sometimes, a laparoscopic surgery is needed to confirm the diagnosis.
Treatment for endometriosis includes pain management, hormone therapy, and sometimes surgery. The goal is to ease symptoms, slow the disease, and improve life quality. While there’s no cure, managing the condition can help women with menstrual disorders and reproductive health.
“Endometriosis is a chronic, painful condition that can have a significant impact on a woman’s quality of life. It’s important for women to be aware of the symptoms and seek medical attention if they suspect they may have this condition.”
Medical Treatments and Interventions for Menstrual Disorders
Medical professionals have many ways to treat menstrual disorders. They use hormonal therapy and surgery, depending on the patient’s needs.
Hormonal Therapy Options
Hormonal therapy is a common treatment for menstrual issues. It includes oral contraceptives, progestin-only pills, and other supplements. These help balance hormones, regulate cycles, and ease symptoms.
- Oral contraceptives: These pills can make the cycle regular and lessen cramps and heavy bleeding.
- Progestin-only medications: These, like medroxyprogesterone acetate, treat endometriosis and fibroids, which can cause menstrual problems.
- Hormone supplements: Estrogen or testosterone may be given to fix hormonal imbalances that lead to irregular periods.
Surgical Interventions When Necessary
Surgery is sometimes needed to fix menstrual disorders. Procedures include:
- Endometrial ablation: This removes or destroys the uterine lining to reduce bleeding.
- Myomectomy: Removing fibroids can stop heavy bleeding, pain, and irregular cycles.
- Hysterectomy: Removing the uterus might be needed for severe menstrual issues or other problems.
Choosing the right treatment depends on the patient’s symptoms, causes, and health. A healthcare provider will help decide the best plan.
| Treatment Option | Description | Potential Benefits |
|---|---|---|
| Oral Contraceptives | Combined hormonal pills that regulate the menstrual cycle | Reduce menstrual symptoms, regulate cycle |
| Progestin-only Medications | Medications that target hormonal imbalances | Treat conditions like endometriosis, uterine fibroids |
| Hormone Supplements | Estrogen, testosterone, or other hormonal supplements | Address specific hormonal imbalances |
| Endometrial Ablation | Removal or destruction of the uterine lining | Reduce heavy or prolonged bleeding |
| Myomectomy | Surgical removal of uterine fibroids | Alleviate symptoms like heavy bleeding, pain, irregular cycles |
| Hysterectomy | Removal of the uterus | Address chronic, severe menstrual disorders |
Natural Remedies and Lifestyle Changes for Managing Menstrual Health
Managing menstrual health can be helped by natural remedies and lifestyle changes. These include dietary adjustments, physical activities, and alternative therapies. They can ease symptoms and improve overall well-being.
Dietary changes are a key step. Adding herbs, spices, and whole foods can balance hormones and reduce inflammation. For example, ginger, turmeric, and omega-3 foods like flaxseeds and walnuts can ease cramps and PMS symptoms.
Lifestyle changes also play a big role. Regular exercise, like yoga or brisk walking, can manage stress and reduce symptoms. Stress-management techniques, such as meditation, can also help regulate the menstrual cycle.
Alternative therapies, like acupuncture and herbal medicine, can offer relief. These holistic approaches aim to solve the root cause of problems, not just treat symptoms.
| Natural Remedies | Lifestyle Changes |
|---|---|
| Ginger Turmeric Omega-3 rich foods Herbal supplements | Regular exercise Stress management techniques Adequate sleep and rest Hydration and nutrition |
Combining natural remedies and lifestyle changes can help manage menstrual health. This approach can alleviate symptoms of menstrual disorders. Always consult a healthcare professional to find the best plan for you.
“Empowering women to take charge of their menstrual health through natural and holistic means can have a transformative impact on their overall well-being.”
Prevention Strategies and Regular Monitoring
Good menstrual health is key to feeling your best. By using prevention strategies and checking your health often, you can manage your reproductive health. This helps catch any problems early.
Early Warning Signs
Knowing the early signs of menstrual issues is important. Look out for:
- Irregular or unpredictable menstrual cycles
- Excessive bleeding or pain during menstruation
- Missed or delayed periods
- Significant changes in the flow or duration of periods
- Persistent spotting between periods
Acting fast on these signs can prevent bigger problems. It also boosts your chances of getting the right treatment.
When to Seek Medical Help
If your menstrual cycle or reproductive health changes, see a doctor. Look out for these signs:
- Missed periods for three consecutive cycles or more
- Severe menstrual cramps or pain that interferes with daily activities
- Excessive bleeding that lasts for more than a week
- Sudden or unexplained changes in the frequency, duration, or flow of your periods
- Persistent spotting or abnormal vaginal discharge
By watching your menstrual health and tackling any issues, you’re taking important steps. This ensures a healthier approach to your reproductive well-being.
Conclusion
In this guide, we’ve looked into menstrual disorders in detail. We covered everything from the basics of the menstrual cycle to the different conditions that can affect it. We talked about postponement of menstruation and menstrual disorders, their causes, symptoms, and how to manage them.
It’s important to understand the menstrual cycle and its possible problems for reproductive health. By noticing early signs and getting medical help, women can tackle menstrual disorders and avoid serious issues. It’s key to keep an eye on your health, make lifestyle changes, and work with doctors.
As we wrap up, we urge all women to focus on their menstrual health. Don’t be afraid to ask for help if you notice any issues or irregularities. By learning and taking care of ourselves, we can handle the menstrual cycle’s challenges and take back control of our reproductive health.
FAQ
Q: What is the difference between amenorrhea and oligomenorrhea?
A: Amenorrhea means you don’t get your period at all. Oligomenorrhea is when your periods are infrequent or irregular. Both are menstrual issues with different causes.
Q: How can hormonal imbalances lead to postponement of menstruation?
A: Hormonal problems, like in PCOS or thyroid issues, can mess up your menstrual cycle. This often leads to late or missed periods.
Q: What are the main causes of primary amenorrhea?
A: Primary amenorrhea can come from genetic or physical issues, like birth defects. Hormonal problems, like those from the pituitary or ovaries, also play a role.
Q: How can stress affect menstrual cycles?
A: Stress can mess with the hormones that control your period. This can cause irregularities, like late or missed periods.
Q: What is the link between endometriosis and menstrual disorders?
A: Endometriosis, where uterine lining grows outside the uterus, can cause painful periods and heavy bleeding. It also leads to irregular periods, like delayed menstruation.
Q: What are the common treatment options for menstrual disorders?
A: Treatments often include hormonal therapy, like birth control pills or hormone meds. Sometimes, surgery is needed too.
Q: How can natural remedies and lifestyle changes help manage menstrual health?
A: Healthy habits, like a balanced diet and exercise, can help. Stress management also plays a big role in menstrual health.
Q: When should someone seek medical attention for menstrual irregularities?
A: See a doctor if your periods are always late, missing, or if you have other symptoms. These could mean you need medical help.
