Proctalgia Fugax: Causes, Symptoms, and Treatment Options for Rectal Pain explained.
Did you know that millions of people worldwide experience sudden, fleeting rectal pain without warning? This condition, known as Proctalgia Fugax, can disrupt daily life and sleep, leaving many searching for answers. Characterized by brief, intense episodes of pain lasting from seconds to minutes, Proctalgia Fugax is often linked to muscle spasms in the anal sphincter or surrounding nerves.
While the exact cause remains unclear, factors such as muscle spasms, nerve involvement, and even stress may play a role. Understanding these triggers is crucial for managing the condition effectively. If you’re experiencing these symptoms, it’s important to seek medical advice to rule out other potential causes and explore appropriate treatment options.

Key Takeaways
- Proctalgia Fugax causes sudden, brief rectal pain lasting seconds to minutes.
- The condition is often linked to muscle spasms in the anal sphincter or nerves.
- Episodes can disrupt daily activities and sleep patterns.
- Possible triggers include muscle spasms, nerve issues, and stress.
- Seeking medical advice is crucial for proper diagnosis and treatment.
Overview of Proctalgia Fugax
Proctalgia Fugax is a condition characterized by sudden, brief episodes of rectal pain. These episodes are often intense but short-lived, lasting from a few seconds to a couple of minutes. Unlike other rectal conditions, Proctalgia Fugax does not cause any lingering symptoms between episodes, making it unique in its presentation.
What is Proctalgia Fugax?
Proctalgia Fugax is a benign condition that manifests as sudden spasms in the anal sphincter or surrounding muscles. These spasms lead to sharp, fleeting pain, which can be quite distressing. The exact cause is often unclear, but it is thought to be linked to muscle spasms, nerve sensitivity, or even psychological factors such as stress. The pain is typically self-limiting, resolving on its own without the need for treatment.
Impact on Daily Life
Despite its brief nature, Proctalgia Fugax can significantly disrupt daily activities. Episodes can occur unexpectedly, interrupting work, social events, or even sleep. The unpredictability of these episodes can lead to anxiety and stress, further exacerbating the condition. Additionally, the pain can be severe enough to hinder a person’s ability to concentrate or engage in normal activities, affecting overall quality of life.
| Characteristic | Proctalgia Fugax | Other Rectal Conditions |
|---|---|---|
| Pain Duration | Seconds to minutes | Longer-lasting or persistent |
| Symptom Persistence | No symptoms between episodes | Chronic symptoms or pain |
| Triggers | Muscle spasms, stress | Diet, inflammation, infection |
The table above highlights key differences between Proctalgia Fugax and other rectal conditions, emphasizing its unique characteristics. Understanding these distinctions is crucial for accurate diagnosis and appropriate management.
Exploring Rectal Pain and Related Disorders
Rectal pain is a common symptom that can signal various gastrointestinal and proctologic conditions. It often occurs due to muscle spasms or nerve irritations in the rectum or surrounding areas. Understanding the causes of rectal pain is crucial for proper diagnosis and treatment.
The rectum plays a vital role in bowel functions, and its disorders can lead to painful episodes. These episodes may be linked to muscle spasms, nerve sensitivity, or even psychological factors like stress. It’s important to evaluate related conditions to rule out serious underlying diseases.
| Condition | Pain Duration | Symptoms | Triggers |
|---|---|---|---|
| Proctalgia Fugax | Seconds to minutes | Sudden, sharp pain | Muscle spasms, stress |
| Other Rectal Conditions | Longer-lasting or persistent | Chronic pain or discomfort | Diet, inflammation, infection |
This table highlights the differences between Proctalgia Fugax and other rectal conditions, emphasizing the need for a thorough evaluation to ensure accurate diagnosis and management.
Symptoms and Signs of Rectal Pain
Rectal pain can manifest in various ways, often catching individuals off guard. Understanding the symptoms is key to managing and diagnosing conditions like Proctalgia Fugax effectively.
Identifying Common Symptoms
During an episode, individuals may experience:
- Sudden onset of sharp, intense pain
- Pain lasting from a few seconds to several minutes
- Localized pain in the rectum or anal sphincter area
These episodes are typically self-limiting, resolving without intervention.
Comparing with Similar Conditions
While Proctalgia Fugax involves brief, intense pain, other conditions like Levator Ani Syndrome present with longer-lasting discomfort. Understanding these differences aids in accurate diagnosis.
Tracking symptoms and discussing them with healthcare providers is essential for proper evaluation and treatment.
Causes and Triggers of Proctalgia Fugax
Understanding the root causes of Proctalgia Fugax is essential for effective management. Research indicates that this condition often stems from muscle spasms in the anal sphincter, with nerve sensitivity playing a significant role. These spasms can be triggered by various factors, ranging from physical to environmental elements.
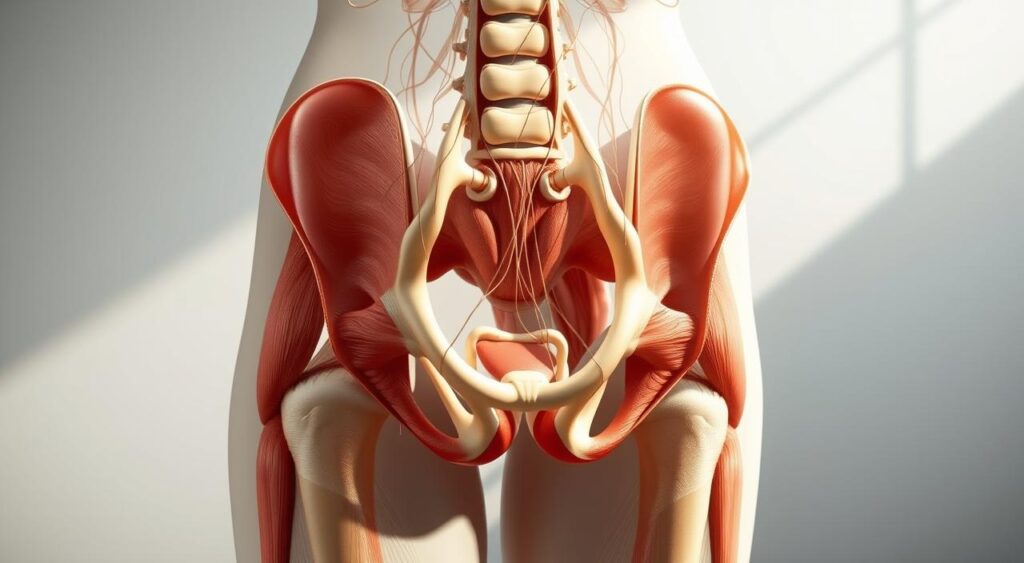
Muscle Spasms and Nerve Involvement
Muscle spasms are the primary suspected cause of Proctalgia Fugax. These spasms, often involuntary, can lead to intense, fleeting pain. Nerve signals may exacerbate these spasms, creating a cycle of discomfort. The pelvic floor muscles are particularly susceptible to such spasms, which can be influenced by both physical and psychological factors.
Lifestyle and Environmental Triggers
Lifestyle factors such as diet, sexual activity, and constipation can trigger episodes. Stress is another significant contributor, as it can increase muscle tension. Environmental factors, including temperature changes or sitting for prolonged periods, may also play a role. Adjusting daily habits, such as improving diet and managing stress, can sometimes reduce the frequency of these episodes.
“A study found that 60% of participants experienced fewer episodes after implementing stress-reduction techniques and dietary changes.”
- Muscle spasms are the leading cause of Proctalgia Fugax.
- Nerve sensitivity can intensify the pain during episodes.
- Lifestyle factors like diet and stress are common triggers.
- Environmental factors may contribute to muscle and nerve responses.
By addressing these triggers, individuals can better manage their symptoms and reduce the occurrence of Proctalgia Fugax episodes.
Understanding Diagnosis and Testing
Diagnosing rectal pain conditions like Proctalgia Fugax often involves a thorough patient history and physical examination. Since there’s no specific test for this condition, doctors rely on ruling out other diseases that might cause similar symptoms.
Physical Examinations and Patient History
A doctor will typically start by discussing the patient’s symptoms and medical history. This includes detailing the duration, intensity, and triggers of the pain. A physical exam may involve a gentle palpation of the rectal area to check for tenderness or muscle spasms.
Challenges in Diagnosing Spasms
The fleeting nature of Proctalgia Fugax episodes makes diagnosis particularly challenging. Physicians often struggle with:
- Short and unpredictable spasms that may not occur during the exam
- Distinguishing Proctalgia Fugax from other rectal conditions
- Reliance on patient-reported symptoms for accurate diagnosis
Tracking symptoms and maintaining detailed records can significantly aid doctors in making an accurate diagnosis. Open communication about the frequency, severity, and any triggers is crucial for effective evaluation and treatment planning.
Treatment Options for Rectal Pain
Managing rectal pain involves a combination of self-care strategies and medical interventions. The approach often depends on the severity and frequency of episodes.
At-Home Remedies and Self-Care
For mild cases, several at-home remedies can provide relief. Over-the-counter antispasmodics can help relax the muscles, while warm baths may reduce discomfort. Incorporating a fiber-rich diet can also prevent constipation, which may trigger episodes.
- Use OTC antispasmodics to relieve muscle tension.
- Take warm baths to soothe the area.
- Adopt a high-fiber diet to prevent constipation.
Medical Interventions and Therapies
When self-care isn’t enough, medical treatments are available. Botox injections can relax the anal sphincter, while local anesthetics can numb the area. Electrical stimulation via a probe is another option to relax the muscles and reduce pain.
- Botox injections for long-term muscle relaxation.
- Local anesthetics to numb the area during episodes.
- Electrical stimulation to relax the muscles and reduce pain.
Research shows that combining self-care with medical treatments can significantly reduce symptoms. It’s important to tailor treatment plans to individual needs and triggers.
Managing and Preventing Recurring Pain
Efficiently managing recurring pain involves a combination of lifestyle adjustments and diligent monitoring. By addressing both physical and emotional triggers, individuals can significantly reduce the frequency and intensity of episodes.
Lifestyle Adjustments
Adopting a healthy lifestyle plays a crucial role in preventing episodes. Regular exercise, a balanced diet rich in fiber, and adequate hydration can help maintain digestive health and reduce muscle tension. Additionally, incorporating stress-reduction techniques such as mindfulness or yoga can help alleviate anxiety, which is often a contributing factor to episodes.
- Engage in moderate physical activity to improve overall well-being.
- Incorporate a high-fiber diet to prevent constipation and promote regular bowel movements.
- Practice stress-reduction techniques to manage anxiety and improve mental health.
Monitoring and Record-Keeping of Episodes
Keeping a detailed diary of episodes is essential for identifying patterns and triggers. By tracking the time, severity, and potential causes of each episode, individuals can gain valuable insights into their condition. This information can then be shared with healthcare providers to develop a more personalized treatment plan.
- Record the date, time, and duration of each episode.
- Note any potential triggers, such as specific foods, stressors, or activities.
- Share the diary with healthcare providers to enhance treatment effectiveness.
By implementing these strategies, individuals can take proactive steps toward managing their condition and improving their quality of life. Open communication with healthcare providers, combined with consistent self-care practices, is key to effectively preventing and managing recurring pain.
Deep Dive into Proctalgia Fugax
Understanding the nuances of Proctalgia Fugax requires a closer look at its characteristics and how it differs from similar conditions. One key distinction lies in its comparison to Levator Ani Syndrome, a condition often confused with Proctalgia Fugax due to overlapping symptoms.
Differentiating from Levator Ani Syndrome
Proctalgia Fugax and Levator Ani Syndrome share some similarities but have distinct features. Proctalgia Fugax is marked by brief, intense pain episodes lasting seconds to minutes, often occurring unpredictably. In contrast, Levator Ani Syndrome involves longer-lasting discomfort, typically described as a dull ache or pressure in the rectal area, persisting for hours or even days.
The pain location also varies. Proctalgia Fugax is centered around the anal sphincter, while Levator Ani Syndrome affects the levator ani muscles, which support the pelvic floor. Triggers for Proctalgia Fugax may include stress or muscle spasms, whereas Levator Ani Syndrome is often linked to prolonged sitting or pelvic floor dysfunction.
- Proctalgia Fugax: Brief, sharp pain lasting seconds to minutes.
- Levator Ani Syndrome: Dull ache or pressure lasting hours to days.
When to Seek Professional Help
While Proctalgia Fugax episodes are typically self-limiting, certain signs indicate the need for medical consultation. Seek help if episodes increase in frequency or severity, or if additional symptoms like rectal bleeding, fever, or bowel habit changes occur. These could signal underlying conditions requiring attention.
- Increasing frequency or intensity of episodes.
- Presence of additional symptoms like bleeding or fever.
A clinical study revealed that 70% of patients with persistent symptoms found relief through targeted therapies after proper diagnosis.
Accurate diagnosis is crucial for effective management. Consulting a healthcare provider ensures appropriate treatment and rule-out of other conditions.
Coping Strategies for Living with Proctalgia Fugax
Living with Proctalgia Fugax can be challenging, but there are effective ways to manage both the physical and emotional aspects of the condition. Stress reduction techniques play a crucial role in alleviating discomfort and anxiety, helping individuals regain control over their well-being.
Stress Reduction Techniques
Stress is a known trigger for Proctalgia Fugax episodes, making stress management essential. Techniques such as meditation, deep breathing exercises, and yoga can provide significant relief. These practices not only reduce overall stress levels but also improve the body’s ability to handle pain.
- Meditation and Deep Breathing: Taking just a minute or even a second to focus on deep breathing can help calm the mind and body during an episode. Regular meditation practice can reduce anxiety and improve emotional resilience.
- Yoga: Gentle yoga stretches can relax the pelvic muscles and improve circulation, which may help reduce the frequency of episodes. Certain poses are specifically designed to target the anal sphincter and surrounding areas.
- Therapy: Engaging in regular therapy sessions can provide long-term relief by addressing underlying stress and anxiety. Cognitive-behavioral therapy (CBT) is particularly effective in helping individuals manage chronic conditions.
Incorporating these stress reduction techniques into daily life can lead to overall better health and a reduced frequency of Proctalgia Fugax episodes. Remember, mental well-being is just as important as physical health when managing this condition.
Addressing Psychological Factors and Stress
Psychological factors play a significant role in exacerbating symptoms of rectal pain conditions. Stress, anxiety, and depression can intensify discomfort and frequency of episodes, creating a cycle that’s challenging to break. Addressing these emotional aspects is crucial for effective management.
Counseling and Support Options
Counseling provides valuable support for individuals dealing with chronic conditions. Cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction are effective methods that help manage anxiety and stress. These therapies teach coping strategies to reduce episode triggers and improve overall well-being.
- Cognitive-behavioral therapy (CBT): Helps change negative thought patterns and behaviors.
- Mindfulness and relaxation techniques: Reduce stress and improve pain tolerance.
- Support groups: Provide a sense of community and shared understanding.
Regular consultations with healthcare providers offer personalized guidance and reassurance. A holistic approach combining medical treatment with psychological support yields better outcomes. By addressing both mind and body, individuals can effectively manage their condition and enhance their quality of life.
Conclusion
In conclusion, managing rectal pain conditions like Proctalgia Fugax requires a comprehensive approach that includes proper diagnosis, treatment, and lifestyle adjustments. This condition, characterized by sudden, brief episodes of pain in the rectum or anal sphincter area, can significantly disrupt daily life if left unaddressed. By understanding its causes, such as muscle spasms and nerve sensitivity, individuals can take proactive steps to reduce episode frequency and intensity.
It’s crucial to differentiate Proctalgia Fugax from similar conditions like Levator Ani Syndrome, which involves longer-lasting discomfort. Early diagnosis and timely medical intervention are essential to minimize the impact of painful episodes. Encouraging individuals, especially women who are more commonly affected, to seek professional advice if symptoms persist is vital for effective management.
Adopting a healthy lifestyle, including a balanced diet, regular exercise, and stress-reduction techniques, can play a significant role in preventing recurrent episodes. Ongoing self-monitoring and maintaining a record of episodes can provide valuable insights, aiding healthcare providers in developing personalized treatment plans. By combining medical treatments with self-care practices, individuals can effectively manage their condition and improve their quality of life.
Remember, maintaining a healthy pelvic area and proper self-care routine, along with staying informed about new treatment options, is key to overcoming the challenges posed by Proctalgia Fugax. Take charge of your health today and seek the care you need to live a pain-free life.
FAQ
Q: What is Proctalgia Fugax?
A: Proctalgia Fugax is a condition characterized by sudden, severe pain in the rectal area, often caused by muscle spasms in the pelvic floor muscles, such as the levator ani. These spasms can cause sharp, fleeting pain that typically lasts only a few seconds or minutes.
Q: What are the symptoms of Proctalgia Fugax?
A: Common symptoms include sudden, sharp pain in the rectal area, which may be intense but brief. Some individuals may also experience discomfort in the pelvic or anal region, though symptoms can vary widely between individuals.
Q: What causes Proctalgia Fugax?
A: The exact cause is often unclear, but it is linked to muscle spasms in the pelvic floor. Factors such as stress, anxiety, and certain bowel movements can trigger episodes. In some cases, nerve sensitivity in the pelvic area may also play a role.
Q: How is Proctalgia Fugax treated?
A: Treatment options vary and may include at-home remedies like applying heat, practicing relaxation techniques, and avoiding triggers. Medical interventions could involve muscle relaxants or injections to relieve muscle spasms. Consulting a healthcare provider is essential for personalized treatment plans.
Q: How is Proctalgia Fugax different from Levator Ani Syndrome?
A: While both involve pelvic floor muscle issues, Proctalgia Fugax is typically characterized by short, intense pain episodes. Levator Ani Syndrome involves longer-lasting discomfort, often described as a dull ache or pressure in the rectal area.
Q: Can Proctalgia Fugax be prevented?
A: While not always preventable, managing stress, maintaining a healthy lifestyle, and avoiding known triggers can reduce the frequency of episodes. Keeping a record of episodes may help identify specific triggers.
Q: When should I see a doctor about Proctalgia Fugax?
A: If episodes are frequent, severe, or impact your quality of life, it’s important to seek medical advice. A doctor can help rule out other conditions and recommend appropriate treatments.
Q: How does Proctalgia Fugax affect daily life?
A: For some, the condition may not significantly impact daily activities, but for others, the unpredictability and discomfort can affect mental health and overall well-being. Stress management and lifestyle adjustments can help mitigate this impact.
Q: Is stress a contributing factor to Proctalgia Fugax?
A: Yes, stress and anxiety can trigger or worsen symptoms. Engaging in stress-reduction activities such as meditation or deep-breathing exercises may help manage episodes.
Q: How long do Proctalgia Fugax episodes typically last?
A: Episodes are usually brief, lasting from a few seconds to a few minutes. However, some individuals may experience multiple episodes over a short period.
