Learn about Pulmonary Embolism, including symptoms, causes, treatments, and risks. Equip yourself with essential information for proactive health management.
This issue can hit anyone, but some are at higher risk. Health problems or a sedentary lifestyle can increase your chances. Spotting the signs early is crucial. Quick action can save lives, and many people recover fully after treatment.

Key Takeaways
- Pulmonary embolism can affect people from different age groups.
- Blood clots can travel to the lungs and cause sudden breathing issues.
- Early detection helps prevent serious complications.
- Staying active can lower your chance of developing a dangerous clot.
- Prompt medical care boosts the odds of a full recovery.
Understanding Pulmonary Embolism Symptoms
Many people suddenly feel out of breath, but they might not think it’s a clot. Sharp chest pain that gets worse when you breathe in is a big warning sign. Feeling dizzy or faint could mean there’s a problem with blood flow.
Feeling very tired and having a fast heartbeat can be signs of pe. Some notice their chest feels tight, which might seem like a minor issue. But being alert to these changes can help you act fast.
Early Warning Signs of a Blood Clot in Lungs
Spotting early signs can help avoid ignoring serious problems. Feeling intense pressure in your ribcage or sudden breathlessness are common warnings. If you cough up blood, you need to see a doctor right away.
Recognizing Pulmonary Emboli in Different Age Groups
Teenagers might feel a bit off or tired, while adults often face severe chest pain and fast breathing. Older people might feel confused or very weak. Each age group shows different symptoms when a pe happens, making early detection crucial.
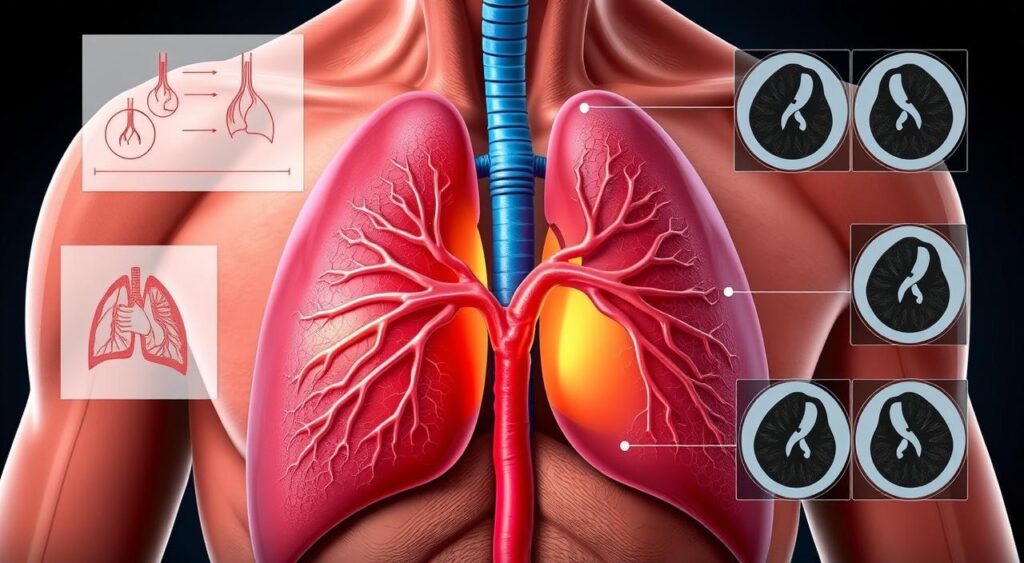
Pulmonary Embolism
Pulmonary embolism is a serious condition. It happens when a clot blocks blood flow in the lungs. Often, this clot starts in the leg veins and moves up, causing trouble with oxygen exchange.
Signs can pop up without warning, and everyone’s experience is different. Some feel sudden chest pressure, while others notice they’re breathing faster. This blockage puts extra strain on the heart and disrupts normal circulation.
Experts say to seek help right away if you have unexplained breathlessness or discomfort. The goal of treatment is to dissolve or remove the clot. A blood clot in the lungs needs quick attention from doctors.
- Clot Formation: Tends to originate in the legs or pelvis.
- Impact: Alters oxygen levels by constricting airflow.
| Factor | Description | Possible Outcome |
|---|---|---|
| Clot Origin | Veins in the legs | Travel to pulmonary artery |
| Severity | Size of the blockage | Ranging from mild to life-threatening |
| Response | Rapid intervention | Improves future lung function |
Common Causes and Risk Factors
Blood clots can form in deep veins when blood flow slows down or the body stays still for too long. These clots can move to the lung, causing pulmonary emboli that block blood flow. Traveling for a long time or staying in bed can increase the risk. Some people are more likely to get clots because of their genes.
Smoking and some health conditions can make it harder for the body to prevent blood clots. Being inactive or having poor health can also make you more at risk. To prevent clots, it’s important to stay active and get regular health check-ups.
PE and Deep Vein Thrombosis
Deep Vein Thrombosis (DVT) is a big cause of blood clots. Clots often start in the legs and then move to the lungs. This can block the flow of oxygen, which is vital for breathing.
Role of Pulmonary Artery Embolism in Patient Vulnerability
When a clot gets stuck in the pulmonary artery, it can make breathing harder and cause chest pain. Being still for a long time or having surgery recently can make this more likely. This can lead to serious health problems.
| Risk Factor | Possible Impact | Suggested Prevention |
|---|---|---|
| Prolonged Sitting | Reduced Blood Circulation | Frequent Walk Breaks |
| Genetic Tendency | Elevated Clot Risk | Medical Screenings |
| Smoking | Increased Vessel Damage | Quit Programs |
Diagnosis and Medical Evaluations
Spotting clots is crucial in diagnosing a pulmonary artery embolism. Doctors start by looking at a patient’s health history and checking for signs of a blockage. They often ask for blood tests, like a D-dimer test, to see if there’s abnormal clotting.
When D-dimer levels are high or symptoms are concerning, imaging is used. This helps doctors see what’s going on inside the lungs.
CT scans or ventilation-perfusion scans give a clear view of lung blood flow. These tests help doctors make quick decisions. They guide the best treatment plan, helping patients recover faster.
A prompt investigation pinpoints the cause of breathing difficulties and chest discomfort.
| Diagnostic Tool | Focus Area | Benefit |
|---|---|---|
| D-dimer Test | Detect Clot Fragments | Fast and Cost-Effective |
| CT Scan | Identify Pulmonary Blockages | High-Resolution Images |
| V/Q Scan | Examine Air and Blood Flow | Lower Radiation Level |
Treatment Options for Pulmonary Embolism
Quick action is key when dealing with blood clots. Special treatments aim to improve blood flow and reduce symptoms. Care teams create plans tailored to each person, focusing on quick relief and preventing future problems.
Medications and Blood Thinners
Anticoagulants stop clots from getting bigger and protect the lungs. In some cases, drugs dissolve large clots, easing the crisis. Regular check-ups help adjust medications to meet individual needs.
Surgical Interventions
Surgery may be needed to remove big clots through embolectomy. Doctors might also put filters in veins to catch stray clots. These steps offer quick relief when usual treatments don’t work fast enough.
Ongoing Care and Rehabilitation
Regular check-ups are crucial to track progress and lower future risks. These visits might include exercise to build strength and confidence. Rehabilitation programs help improve function, making it safer to go back to daily life.
Preventative Measures
Being aware of daily risks can lower the chance of a clot. Moving often during long flights or desk work helps avoid leg strain. Simple actions like stretching and walking every hour can help a lot.
Checking for genetic conditions is also important. It helps if your family has a higher risk of blood clots. These steps help protect you from future problems.
Doctors might suggest wearing compression stockings or taking certain medicines for those at risk. These steps help keep blood flowing well and prevent clots. It’s good to talk to your doctor about what’s best for you.
- Regular exercise promotes improved circulation.
- Staying hydrated assists in preventing thicker blood consistency.
- Early detection of clotting disorders leads to more targeted care.
| Preventive Tool | Key Benefit |
|---|---|
| Compression Stockings | Enhance leg circulation |
| Blood-Thinning Medications | Lower clot formation risk |
| Genetic Testing | Identify hereditary vulnerabilities |
Lifestyle Factors That Influence PE
Daily routines play a big role in keeping our circulation and health in check. By choosing supportive habits, we help our bodies recover better. This also improves the results of treatments for pulmonary embolism.
Importance of Regular Exercise
Regular exercise is key to a strong heart and lower clot risk. Activities like walking, yoga, or light aerobics keep blood flowing well. It’s important to start slowly and match the exercise to your fitness level for the best results.
Smoking Cessation and Weight Management
Smoking puts extra pressure on our blood vessels and harms our lungs. Quitting smoking can greatly reduce the risk of more clots. It also helps treatments for pulmonary embolism work better.
Keeping a healthy weight through balanced eating and exercise is also crucial. It reduces stress on vital organs. These lifestyle changes help prevent future problems and support better health.
Potential Complications and Long-Term Effects
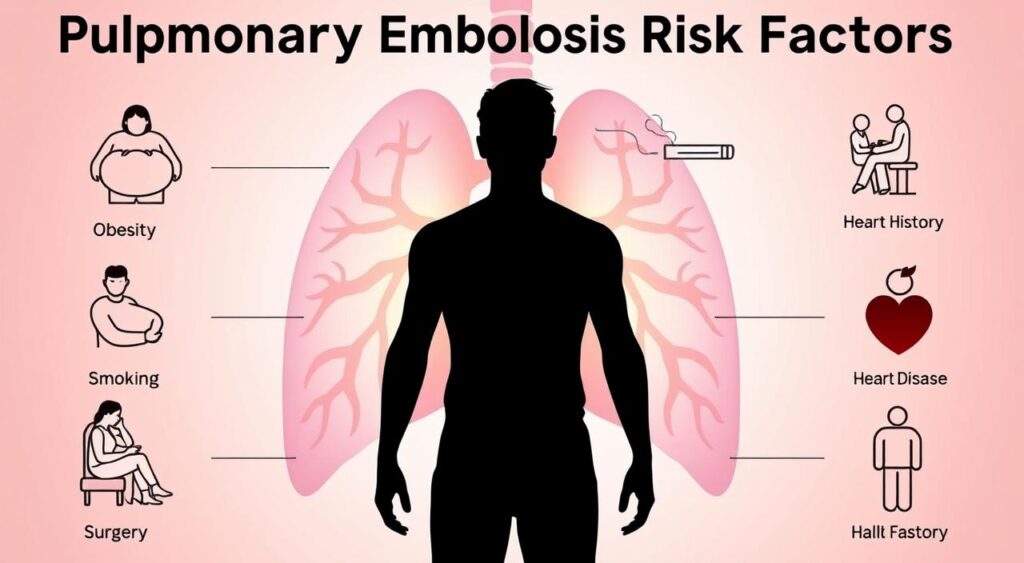
Challenges can last if a clot is not found or if pulmonary embolism risk factors stay the same. Chronic pulmonary hypertension can make the heart work harder. This can make simple tasks hard.
Some people might get pulmonary infarction, which harms lung tissue and causes chest pain. The Mayo Clinic says that repeated clotting harms the lungs and heart. Regular check-ups and scans are key to catching problems early.
“Early detection is vital to help doctors intervene before complications become severe.”
Knowing about pulmonary embolism risk factors helps patients avoid long-term problems. Exercise, regular check-ups, and quick medical care can make a big difference. They help improve health and quality of life.
Myths and Facts About Blood Clots in Lungs
Blood clots in the lungs can affect anyone, not just those with heart problems. Many factors increase the risk. A correct pulmonary embolism diagnosis uncovers these risks.
Some think they’re safe if they’ve never had a clot before. But, a quick medical check can spot early signs. This helps prevent worries from growing.
Debunking Common Misconceptions
Myths spread when we don’t have the facts. One myth is that blood clots always hurt a lot. But, some clots don’t cause pain, making a quick pulmonary embolism diagnosis crucial. Another myth is that only older people get clots. But, younger people can also get them, especially if they’re not active or have certain health issues.
| Myth | Fact |
|---|---|
| Clots only happen to seniors | They can affect various age groups |
| A clot always causes severe pain | Some clots may show mild or no symptoms |
Where to Find Reliable Information
Look to trusted sources like the American Heart Association or Mayo Clinic. They provide up-to-date information on treatments and concerns. Doctors and reliable websites share proven facts to help you stay safe.
Conclusion
Knowing about health issues is the first step to taking care of yourself. Learning about pulmonary embolism can lead to quick action and treatment. This can help avoid serious problems and give people time to heal.
Doctors use advanced tests and blood work to diagnose this condition. Regular health check-ups are important for this reason.
Being active and using prevention methods can help prevent blood clots. The Mayo Clinic advises talking to a doctor about your risk. Being aware can lead to better choices and safer outcomes.
Pulmonary embolism is serious, but with early care, it can be managed. Getting advice from medical experts is a great way to protect yourself and your loved ones. With the right steps, pulmonary embolism can be handled effectively.
FAQ
Q: Are PE and pulmonary emboli the same condition?
A: A PE (Pulmonary Embolism) is usually a single clot in the lungs. Pulmonary emboli can mean multiple clots. Both are serious and need quick medical help.
Q: What causes a blood clot in lungs, also known as a pulmonary artery embolism?
A: A blood clot in lungs often comes from another part of the body, like the legs. This is called deep vein thrombosis (DVT). Things like sitting still for too long, surgery, or genetic issues can help it happen.
Q: What are the most common pulmonary embolism symptoms?
Pulmonary embolism symptoms include sudden shortness of breath and sharp chest pain. You might also feel lightheaded, faint, or cough up blood. These signs need urgent medical attention.
Q: How is a pulmonary embolism diagnosis typically made?
A: A pulmonary embolism diagnosis uses tests like CT scans or V/Q scans. Blood tests, like the D-dimer, also help. Doctors look at these results, your symptoms, and medical history to confirm a PE.
Q: Are there pulmonary embolism risk factors to be aware of?
A: Yes. Big pulmonary embolism risk factors include sitting still for a long time, recent surgeries, and smoking. Being overweight, having heart disease or cancer, and inherited clotting disorders also increase risk.
Q: What does pulmonary embolism treatment usually involve?
Pulmonary embolism treatment starts with blood thinners. For severe cases, clot-busting drugs or surgery might be needed. Recovery often means ongoing medication, regular doctor visits, and lifestyle changes to prevent more clots.
Q: Can lifestyle changes help prevent pulmonary embolism causes?
A: Yes. While some risks are genetic or due to certain conditions, lifestyle changes can help. Regular exercise, a healthy weight, and not smoking can lower your risk. Your doctor might also recommend compression stockings or blood-thinning medication.
