Pulmonary tuberculosis, or TB, is a serious lung disease caused by Mycobacterium tuberculosis. It mainly hits the lungs but can spread to other areas. TB is a big problem worldwide, affecting millions.
It’s important to know the symptoms, causes, and treatments for TB. This helps catch it early and manage it well.
Key Takeaways
- Pulmonary tuberculosis is a respiratory illness caused by the Mycobacterium tuberculosis bacteria.
- It is a global health concern, affecting millions of individuals worldwide.
- Early detection and proper treatment are essential for managing the disease and preventing its spread.
- Symptoms can include cough, chest pain, fever, and weight loss.
- Factors such as environmental conditions, medical conditions, and lifestyle choices can increase the risk of developing TB.
Understanding Pulmonary Tuberculosis: An Overview
Pulmonary tuberculosis (TB) is a serious disease caused by Mycobacterium tuberculosis. It’s a big problem worldwide. Knowing about it helps us fight it better.
What Makes TB a Global Health Concern
TB is a big worry because it affects many people. The World Health Organization says there were 10.6 million new cases of TB in 2021. Also, 1.6 million deaths were linked to TB that year.
The Impact of Mycobacterium Tuberculosis
Mycobacterium tuberculosis is very contagious and mainly hits the lungs. It can also infect other parts of the body. This leads to different types of TB.
Some people have TB that’s not active. This means the bacteria are sleeping. But, active TB causes symptoms and can lead to serious problems.
The effects of Mycobacterium tuberculosis go beyond health. It also hurts society and the economy. TB hits hard on those who are poor, have weak immune systems, or live in crowded places. To tackle TB, we need to tackle it medically and socially.
“Tuberculosis remains one of the world’s deadliest infectious killers. Each day, over 4,100 people lose their lives to TB, and close to 28,000 people fall ill with this preventable and treatable disease.”
– World Health Organization
Early Signs and Common Symptoms of TB Infection
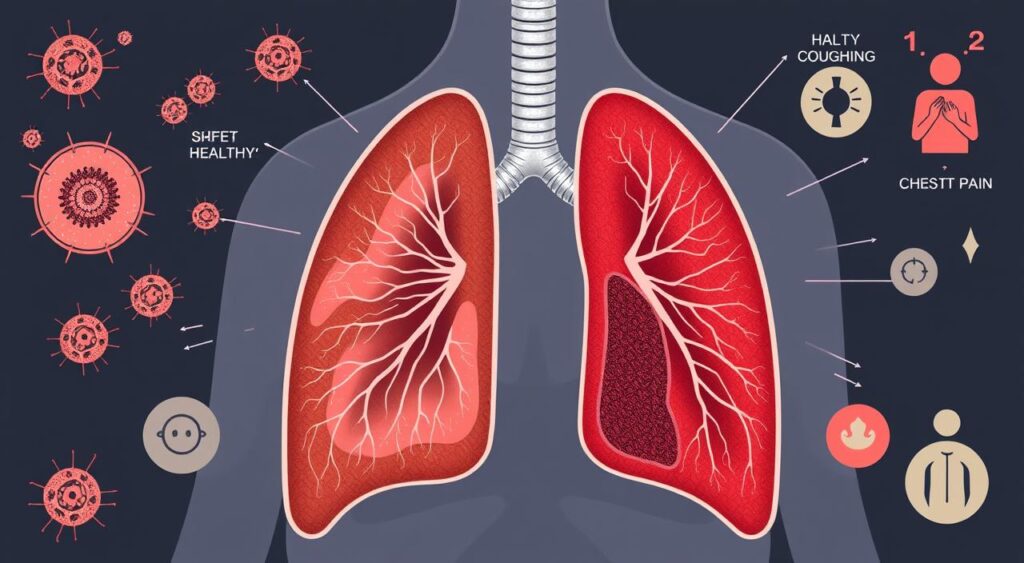
Pulmonary tuberculosis (TB) shows early signs and symptoms that are important to notice. Recognizing these signs early is key for quick diagnosis and treatment. Common symptoms include a chronic cough, chest pain, weight loss, and night sweats.
A persistent cough is often the first sign of TB. This chronic cough may start dry but can lead to coughing up sputum or blood. Chest pain is also common, caused by inflammation and irritation in the lungs.
Unexplained weight loss is another sign of TB. The body’s fight against the bacteria can cause unintentional weight loss. Night sweats are also common, happening during sleep.
“Early recognition of TB symptoms is critical for prompt diagnosis and treatment, which can greatly improve patient outcomes and reduce the risk of transmission to others.”
Seeing these symptoms doesn’t mean you have TB. Similar signs can show up in other diseases. But, a persistent cough, chest pain, weight loss, and night sweats need medical attention.
| Symptom | Description |
|---|---|
| Chronic Cough | A persistent, lingering cough that can be dry or productive of sputum or blood. |
| Chest Pain | Discomfort or pain in the chest area, often due to lung inflammation. |
| Weight Loss | Unexplained, unintentional loss of pounds as the body fights the infection. |
| Night Sweats | Excessive sweating episodes during sleep, a common symptom of TB. |
Knowing the early signs and symptoms of TB helps you act fast. Early treatment can greatly improve health and prevent spreading the disease.

Key Risk Factors and Causes of Pulmonary Tuberculosis
Pulmonary tuberculosis is a serious lung disease caused by Mycobacterium tuberculosis bacteria. Many factors can increase the risk of getting tb infection. Knowing these factors helps us find who is most at risk and how to prevent it.
Environmental Risk Factors
Environmental factors greatly affect the spread and development of pulmonary tuberculosis. Living in crowded, poorly ventilated places raises the risk of TB exposure. Also, areas with poor healthcare and sanitation have more tb cases.
Medical Conditions That Increase TB Risk
Some health conditions weaken the immune system, making TB more likely. HIV/AIDS, diabetes, and malnutrition are examples. They make it harder for the body to fight off TB bacteria.
Lifestyle Factors Contributing to TB
Our lifestyle choices also play a part in TB risk. Smoking, drinking too much alcohol, and being inactive can harm the lungs and overall health. This makes us more susceptible to TB.
| Risk Factor | Description | Relative Risk |
|---|---|---|
| Poverty and Overcrowding | Poor living conditions with limited access to healthcare | 2-5 times higher |
| Malnutrition | Weakened immune system due to nutrient deficiencies | 2-3 times higher |
| Diabetes | Impaired immune response and increased susceptibility | 2-3 times higher |
| Smoking | Damage to the respiratory system and increased risk of infection | 2-3 times higher |
Understanding these risk factors helps us fight pulmonary tuberculosis better. Healthcare workers and public health teams can create better prevention and treatment plans.
How Tuberculosis Spreads: Transmission Patterns
Tuberculosis, or tb infection, is a contagious respiratory illness caused by Mycobacterium tuberculosis bacteria. Knowing how it spreads is key to stopping it. We’ll look at the main ways tb infection spreads and what affects its spread.
The main way tb infection spreads is through the air. When someone with active TB coughs, sneezes, or talks, they release TB bacteria into the air. These tiny particles can be breathed in by nearby people, causing tb infection in those who are at risk.
- Being close to someone with TB for a long time raises the risk of getting infected.
- Living in crowded places, bad air circulation, and not having access to healthcare help TB spread fast.
- Having certain health issues, like HIV/AIDS, makes it harder for the body to fight off TB.
Not everyone who gets exposed to TB will get sick. Sometimes, the body can fight off the infection and keep it from spreading. But, people with latent TB can still get sick if their immune system weakens.

Understanding how TB spreads helps health experts and public health officials fight it. They focus on early detection, treatment, and teaching people about hygiene and how to prevent TB from spreading through the air.
Diagnostic Methods and Testing Procedures
Diagnosing pulmonary tuberculosis (TB) needs a detailed approach. This includes various testing methods. Healthcare experts use different tools to find and confirm TB infection.
Skin Tests and Blood Tests
The Mantoux tuberculin skin test is a common TB diagnostic tool. It involves injecting tuberculin protein under the skin. Then, the area is checked for a reaction after 48-72 hours. A positive result means TB antibodies are present, showing a possible infection.
Blood tests like the interferon-gamma release assay (IGRA) are also used. These tests check the body’s immune response to TB-specific antigens. They offer a more precise TB infection assessment.
Imaging Studies and Culture Tests
Imaging like chest X-rays and CT scans are key in diagnosing pulmonary TB. They help spot the disease’s characteristic lesions and abnormalities. This information helps healthcare providers make the right decisions.
Mycobacterial culture tests are the top choice for confirming TB. They grow samples from the respiratory system in a lab. This confirms the presence of the TB-causing bacteria.
Modern Diagnostic Technologies
- Nucleic acid amplification tests (NAATs): These rapid molecular tests can detect TB bacteria genetic material. They give results in hours, not weeks.
- Whole-genome sequencing: This advanced method analyzes the TB bacteria’s complete genetic makeup. It helps identify the bacteria and test drug effectiveness.
- Artificial intelligence-based algorithms: New AI tools can analyze medical images, like chest X-rays. They help spot TB early and accurately.
Using both old and new diagnostic methods is vital. It helps find tb infection quickly and accurately. This allows healthcare providers to start the right treatment and manage the disease effectively.
Treatment Options and Medication Protocols
Pulmonary tuberculosis (TB) is a complex disease needing a detailed treatment plan. The main goal is to get rid of the Mycobacterium tuberculosis bacteria and stop resistance to antibiotics. Doctors use a mix of antibiotics and watch the patient closely during treatment.
Standard TB Treatment Regimen
The usual treatment for pulmonary TB includes four antibiotics: isoniazid, rifampin, pyrazinamide, and ethambutol. The first two months are the “intensive phase.” During this time, the patient takes all four medicines to kill the TB bacteria.
After the first two months, the “continuation phase” starts. It lasts four to seven months. In this phase, the patient takes isoniazid and rifampin to make sure all TB bacteria are gone and to prevent coming back.
Challenges with Antimicrobial Resistance
Antimicrobial resistance (AMR) is a big problem in treating pulmonary tuberculosis. Some TB strains resist the first-line antibiotics, making treatment harder. Doctors might then use second-line medicines, which can have more side effects and take longer to work.
| Treatment Regimen | Duration | Antibiotics Included |
|---|---|---|
| Intensive Phase | 2 months | Isoniazid, rifampin, pyrazinamide, ethambutol |
| Continuation Phase | 4-7 months | Isoniazid, rifampin |
It’s very important for patients to stick to their treatment plan. They must take all the antibiotics as prescribed, even if they start feeling better. Not finishing the treatment can lead to drug-resistant TB, making it harder to treat in the future.
“The development of antimicrobial resistance in Mycobacterium tuberculosis is a growing global health concern, as it can compromise the effectiveness of current treatment options and lead to more severe and difficult-to-treat forms of the disease.”
Preventing TB Transmission and Spread
Tuberculosis (TB) is a serious health issue that needs a team effort to stop. To fight tb infection, we must use public health measures and personal prevention strategies together.
Public Health Measures
Healthcare and governments are key in stopping TB. They use many prevention strategies. Some important steps include:
- Improving disease tracking and finding TB early
- Offering affordable TB tests and treatments
- Ensuring people get the right TB treatment
- Funding new TB tests, vaccines, and treatments
- Using special public health measures in areas with a lot of TB, like tracing contacts and finding cases
Personal Prevention Strategies
People can also help stop TB. Here are some ways:
- Keeping your mouth and nose covered when you cough or sneeze, and wearing masks in crowded places
- Living a healthy life with good food, exercise, and sleep to keep your immune system strong
- Seeing a doctor right away and finishing all treatment if you have TB
- Learning about TB and telling others to help spread awareness and reduce fear
Working together, using public health measures and personal prevention strategies, we can fight TB. This helps keep everyone safe, especially those who are most at risk.
| Public Health Measures | Personal Prevention Strategies |
|---|---|
| Disease surveillance and early detection Accessible screening and diagnostic services Effective treatment administration Investment in research and development Targeted interventions in high-burden communities | Practicing good respiratory hygiene Maintaining a healthy lifestyle Seeking prompt medical attention and completing treatment Educating oneself and others about TB |
Living with TB: Management and Recovery
Living with pulmonary tuberculosis can be tough, but it’s doable. You can manage your condition and get better. We’ll look at how to live with TB, including coping strategies and lifestyle changes.
Coping with the Emotional Toll
Getting a TB diagnosis can be tough, both physically and emotionally. You might feel scared, anxious, depressed, or isolated. It’s important to face these feelings head-on.
Some good ways to cope include:
- Joining a support group to connect with others facing similar experiences
- Practicing stress-reducing techniques such as meditation, yoga, or deep breathing exercises
- Seeking counseling or therapy to process the emotional impact of the diagnosis
Adjusting Lifestyle and Daily Routines
Managing TB means changing your daily life. This might include:
- Prioritizing rest and sleep to support the body’s healing process
- Incorporating a balanced, nutritious diet to boost the immune system
- Maintaining good hygiene practices to prevent the spread of the infection
- Avoiding smoking, alcohol, and other activities that could compromise the recovery process
The Road to Recovery
With the right treatment and sticking to your medication, you can fully recover from TB. Recovery times vary, but you’ll see your symptoms improve. Regular check-ups and support are key to a successful recovery.
| Symptom | Typical Recovery Timeline |
|---|---|
| Cough | 2-4 weeks |
| Fever | 2-4 weeks |
| Weight Gain | 4-8 weeks |
| Chest X-ray Improvement | 4-8 weeks |
By understanding how to manage TB and embracing the recovery process, you can take charge of your health. This improves your overall well-being and quality of life.
“The key to managing pulmonary tuberculosis is a combination of medical treatment, lifestyle adjustments, and a positive mindset. With the right support and resources, recovery is not only possible but can lead to a renewed sense of health and vitality.”
Conclusion
Pulmonary tuberculosis is a big problem worldwide. We need to work together to solve it. Knowing the signs, causes, and risks of TB is key.
Early detection and proper treatment are crucial. This helps stop TB from spreading. It’s important for our health.
We can fight TB by improving public health and teaching people how to prevent it. Awareness and research are vital. They help us create a healthier world.
Let’s stay focused and keep fighting TB. Together, we can improve health outcomes and protect those who are most at risk. This will make our communities better for everyone.
FAQ
Q: What is pulmonary tuberculosis?
A: Pulmonary tuberculosis (TB) is a serious lung disease. It’s caused by the bacterium Mycobacterium tuberculosis. If not treated, it can cause severe symptoms.
Q: What are the common symptoms of pulmonary tuberculosis?
A: Symptoms include a chronic cough, chest pain, weight loss, and night sweats. These symptoms can get worse over time if not treated.
Q: How does tuberculosis spread from person to person?
A: TB spreads through the air when someone with active TB coughs or sneezes. Tiny droplets with the TB bacteria can be inhaled by others.
Q: What are the risk factors for developing pulmonary tuberculosis?
A: Risk factors include living in crowded or poorly ventilated places. Also, conditions like HIV/AIDS, diabetes, and malnutrition can increase the risk.
Q: How is pulmonary tuberculosis diagnosed?
A: Diagnosis involves tests like skin tests, blood tests, imaging studies, and culture tests. These help find the TB bacteria and confirm the diagnosis.
Q: What are the treatment options for pulmonary tuberculosis?
A: Treatment includes a mix of drugs taken for several months. But, resistant TB strains require more complex treatments.
Q: How can the spread of tuberculosis be prevented?
A: Prevention involves early detection, contact tracing, and infection control. Personal hygiene and avoiding close contact with those with TB also help.
