Did you know that acute respiratory distress syndrome (ARDS) affects up to 200,000 Americans each year? It has a mortality rate as high as 40%. This severe condition, along with its precursor, acute lung injury (ALI), is the main topic of this guide. Understanding these respiratory disorders helps healthcare providers and patients face these challenges.
ALI and ARDS are severe conditions that can cause respiratory failure and long-term health issues. In this article, we’ll explore the causes, diagnosis, and new treatments for these emergencies. This guide is for healthcare professionals and those wanting to learn more about ALI and ARDS.

Key Takeaways
- Acute lung injury and acute respiratory distress syndrome are life-threatening respiratory conditions with high mortality rates.
- Understanding the underlying pathophysiology, common causes, and diagnostic criteria is crucial for effective management.
- Prompt recognition and stabilization, along with appropriate ventilation strategies and supportive care, are essential for improving patient outcomes.
- Ongoing research is exploring new treatment approaches, including targeted therapies and innovative ventilation protocols.
- Rehabilitation and psychological support are vital for supporting patients throughout their recovery journey.
What Are Acute Lung Injury and ARDS?
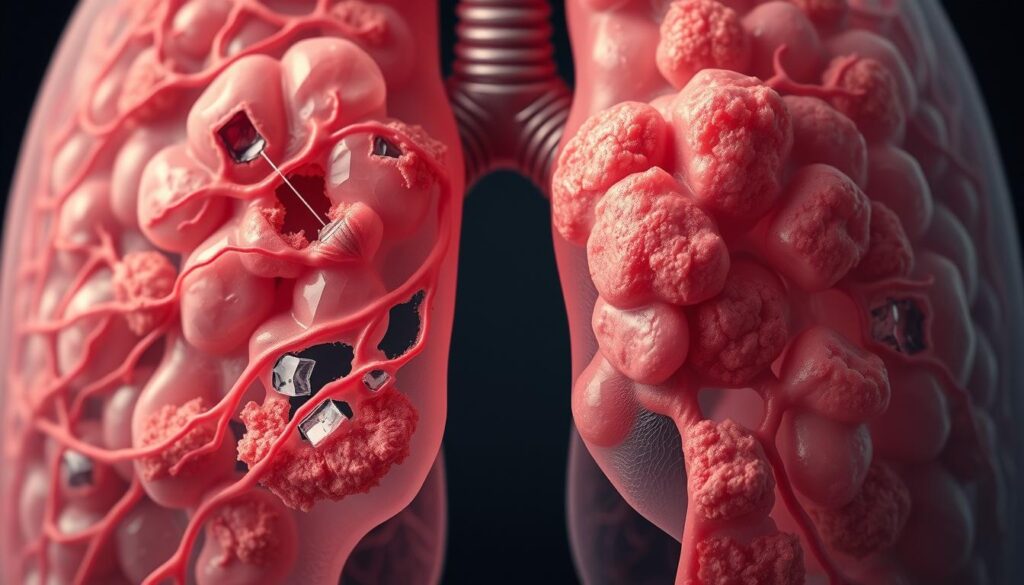
Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) are serious lung conditions. They can cause breathing failure and fluid buildup in the lungs. This makes it hard for the body to get and use oxygen.
Key Characteristics and Definitions
ALI is a lung inflammation and fluid buildup. It leads to poor gas exchange and hypoxemia. ARDS is a more severe version with worse respiratory distress and hypoxia.
Clinical Presentation
- Rapid onset of breathing difficulties and shortness of breath
- Cough, with or without mucus production
- Chest pain or discomfort
- Fever, chills, and signs of infection
- Bluish discoloration of the skin (cyanosis) due to low oxygen levels
Diagnostic Criteria
Doctors use specific criteria to diagnose ALI and ARDS:
| Criteria | ALI | ARDS |
|---|---|---|
| Timing | Acute onset | Acute onset |
| Chest imaging | Bilateral opacities | Bilateral opacities |
| Origin of edema | Not fully explained by cardiac failure or fluid overload | Not fully explained by cardiac failure or fluid overload |
| Oxygenation impairment | Mild to moderate (200 mm Hg | Moderate to severe (PaO2/FIO2 ≤ 200 mm Hg) |
The Pathophysiology Behind Respiratory Failure
At the heart of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) is a complex process. This process leads to severe respiratory failure. It damages the alveolar-capillary barrier, key for gas exchange in the lungs.
Damage to this barrier causes pulmonary edema. This is when fluid builds up in the alveoli. It makes it hard for the lungs to exchange oxygen and carbon dioxide, causing respiratory distress.
Many things can damage this barrier, like inflammation, oxidative stress, and coagulation pathways. These can start from direct or indirect lung injuries. They set off a chain of events that harm the lungs’ function.
It’s important to understand the pathophysiology of respiratory failure in ALI and ARDS. This knowledge helps in creating better treatments and improving patient care. By tackling the causes, healthcare workers can help manage symptoms and fix the alveolar-capillary barrier.
“The pathophysiology of ARDS is a dynamic and multifactorial process that involves complex interactions between the alveolar epithelium, the pulmonary endothelium, and the immune system.”
Common Causes and Risk Factors of ARDS
Acute Respiratory Distress Syndrome (ARDS) can start from many direct and indirect lung injuries. It can also come from conditions that make it more likely to happen.
Direct Lung Injury Causes
Pneumonia is a big cause of ARDS. It’s a serious lung infection that can fill the alveoli with fluid and mess up gas exchange. Other direct lung injuries that can lead to ARDS include:
- Aspiration of gastric contents
- Inhalation of toxic substances
- Lung contusion from chest trauma
- Near-drowning incidents
Indirect Lung Injury Causes
ARDS can also come from indirect lung injuries. For example, severe systemic conditions like sepsis can cause it. Sepsis is a dangerous inflammatory response to infection. It can start a chain of events that leads to ARDS. Other indirect causes of ARDS include:
- Pancreatitis
- Severe burns
- Transfusion-related acute lung injury (TRALI)
Predisposing Conditions
Some conditions can make a person more likely to get ARDS, even with a small lung injury. These conditions include:
- Chronic alcohol abuse
- Diabetes mellitus
- Immunodeficiency disorders
- Liver disease
Knowing the many causes and risk factors of ARDS is key. It helps spot it early, act fast, and manage it well.
Acute Lung Injury and Acute Respiratory Distress Syndrome: Understanding the Connection
Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) are closely related. They both affect respiratory health but have key differences. It’s important to know how they are connected.
ALI often leads to ARDS, which is more severe. ARDS has worse symptoms and affects breathing more. The main difference is the level of lung damage and gas exchange.
ALI patients may have acute onset of respiratory distress, hypoxemia (low oxygen levels in the blood), and bilateral lung opacities on imaging studies. But, the lung injury and breathing problems are less severe than in ARDS.
ARDS, however, has more severe gas exchange problems. This leads to severe hypoxemia and the need for mechanical ventilation. Lung damage in ARDS is more extensive, with a higher risk of long-term complications and death.
The move from ALI to ARDS depends on several factors. These include the cause, initial injury severity, and body’s inflammatory response. Early treatment of ALI is key to preventing ARDS.

Knowing the link between ALI and ARDS helps healthcare professionals. It allows them to provide better care, improving patient outcomes and reducing respiratory failure’s impact.
Diagnostic Approaches and Testing Methods
Diagnosing acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) is complex. It involves imaging studies, lab tests, and blood gas analysis. These tools help find the cause, measure severity, and track how the condition changes.
Imaging Studies
Chest X-rays are key in the early stages of ALI and ARDS. They show signs like bilateral opacities and no big heart. CT scans give more details on lung damage and other issues.
Laboratory Tests
Lab tests are crucial for ALI and ARDS diagnosis. They check for underlying health issues. Biomarkers can also spot ARDS early and help decide treatment.
Blood Gas Analysis
Arterial blood gas (ABG) analysis is vital. It shows how well the lungs are working. Low oxygen and high carbon dioxide levels, with X-ray signs, confirm ARDS.
| Diagnostic Approach | Significance |
|---|---|
| Chest Radiography | Identifies bilateral opacities and absence of cardiomegaly, supporting the diagnosis of ALI and ARDS. |
| Computed Tomography (CT) Scans | Provides detailed information about the pattern and extent of pulmonary edema, as well as associated lung injuries or complications. |
| Laboratory Tests | Helps identify underlying conditions or comorbidities, and may include biomarkers for early detection and risk stratification of ARDS. |
| Arterial Blood Gas (ABG) Analysis | Assesses oxygenation status, carbon dioxide levels, and acid-base balance, key indicators of respiratory dysfunction in ALI and ARDS. |
Using imaging, lab tests, and blood gas analysis together is key. It helps accurately diagnose and manage ALI and ARDS.
The Role of Inflammation in ARDS Development
Acute Respiratory Distress Syndrome (ARDS) is a severe lung condition. It happens when inflammation in the lungs starts quickly. This inflammation is key in ARDS, leading to serious lung damage.
In ARDS, immune cells like neutrophils and macrophages get active. They release harmful substances that damage the lungs. This damage makes it hard for the lungs to breathe properly.
The inflammation in ARDS also harms the lung’s outer layers. This makes it even harder for the lungs to exchange oxygen and carbon dioxide. As a result, the blood may not have enough oxygen, a key symptom of ARDS.
The severity of inflammation in ARDS depends on the cause. For example, injuries like pneumonia cause a strong, local inflammation. But, conditions like sepsis or trauma lead to a more widespread inflammation.
| Inflammatory Mediators in ARDS | Impact on Lung Function |
|---|---|
| Cytokines (e.g., IL-1, IL-6, TNF-α) | Promote inflammation, disrupt alveolar-capillary barrier |
| Chemokines (e.g., IL-8, MCP-1) | Attract and activate immune cells, exacerbate inflammation |
| Proteases (e.g., neutrophil elastase) | Cause direct damage to lung tissue, impair gas exchange |
Understanding inflammation’s role in ARDS is key to better treatment. By focusing on the inflammation, doctors can help reduce the harm caused by ARDS. This can improve the chances of recovery for those with ARDS.
Treatment Strategies and Management Options
Managing Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS) needs a team effort. The main goal is to fix the cause, keep the patient stable, and help the lungs heal. This part talks about the main treatments and care for those with ALI or ARDS.
Initial Stabilization
The first step is to make the patient stable and prevent more lung harm. This includes:
- Using oxygen therapy to boost oxygen levels and ease breathing
- Starting mechanical ventilation to help with breathing and gas exchange
- Managing fluids and blood flow to keep tissues oxygenated
- Fixing the lung injury’s cause, like infections or injuries
Ongoing Care Protocols
Once the patient is stable, the care shifts to ongoing management. This includes:
- Keeping up with mechanical ventilation to protect the lungs
- Using medicines like corticosteroids to calm the immune system
- Supporting the patient with food, physical therapy, and managing side effects
- Watching and changing the treatment plan as needed
Monitoring and Adjustment
Keeping a close eye on the patient and adjusting the treatment is key. Doctors watch the patient’s vital signs, lung function, and how they react to treatments. They make changes to make sure the ARDS treatment is working best for the patient.

With a detailed and flexible treatment plan, doctors hope to better patient outcomes and reduce long-term effects of ALI and ARDS.
Mechanical Ventilation Protocols and Strategies
Mechanical ventilation is key in treating Acute Respiratory Distress Syndrome (ARDS) and respiratory failure. Healthcare teams use different strategies to help patients breathe better. This improves gas exchange during these critical times.
Lung-Protective Ventilation
One main goal in treating ARDS is to use a lung-protective strategy. This method aims to prevent more lung damage. It does this by controlling the amount of air and pressure in the lungs.
By adjusting these settings, doctors can lower the risk of lung injury. This includes barotrauma, volutrauma, and atelectrauma. These conditions can make lung damage worse.
Individualized Ventilation Settings
Every patient with ARDS needs a unique approach to ventilation. Doctors watch closely how the patient responds to the settings. They adjust the fraction of inspired oxygen (FiO2), positive end-expiratory pressure (PEEP), and other settings as needed.
This helps to improve gas exchange and protect the lungs from further damage. It’s all about finding the right balance for each patient.
| Ventilation Strategy | Key Considerations | Potential Benefits |
|---|---|---|
| Lung-Protective Ventilation | Limiting tidal volume and airway pressures | Reduces the risk of barotrauma, volutrauma, and atelectrauma |
| Individualized Ventilation Settings | Adjusting FiO2, PEEP, and other parameters based on patient response | Optimizes gas exchange and minimizes further lung injury |
By using these specific ventilation protocols, healthcare providers can better support ARDS patients. This helps in managing mechanical ventilation, ARDS, and respiratory failure more effectively.

Complications and Associated Conditions
Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) can cause many problems. These issues can happen in the short-term and long-term. It’s important to know about these complications to manage them well.
Short-term Complications
Patients with ALI and ARDS may face several problems early on. Respiratory failure is a big concern, as it can get worse and require a ventilator. Pulmonary edema, or fluid in the lungs, also affects breathing and gas exchange.
Other early issues include:
- Hemodynamic instability, such as low blood pressure or abnormal heart rhythms
- Kidney and liver dysfunction
- Coagulation disorders, leading to increased risk of blood clots
- Infection, including pneumonia and sepsis
Long-term Effects
People who survive ALI and ARDS often deal with lasting effects. ARDS complications can include:
- Decreased lung function and capacity, leading to ongoing respiratory issues
- Muscle weakness and fatigue, which can impair mobility and daily activities
- Cognitive impairment, such as memory problems or difficulty concentrating
- Psychological distress, including anxiety, depression, and post-traumatic stress disorder
Rehabilitation and ongoing care are key to managing these long-term effects. They help patients recover and improve their quality of life.
| Short-term Complications | Long-term Effects |
|---|---|
| Respiratory failure | Decreased lung function |
| Pulmonary edema | Muscle weakness and fatigue |
| Hemodynamic instability | Cognitive impairment |
| Kidney and liver dysfunction | Psychological distress |
| Coagulation disorders | – |
| Infection | – |
Prevention Strategies and Risk Reduction
It’s vital to prevent acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). This is especially true for those at high risk. Healthcare experts can lower the risk of these serious lung problems by tackling the root causes and using specific prevention methods.
Preventing pneumonia is a big step in stopping ALI and ARDS. This can be done through good hand hygiene, flu and pneumococcal vaccines, and ARDS prevention methods like lung-protective ventilation.
Sepsis is another big risk factor for ALI and ARDS. It can be tackled by quickly spotting sepsis and treating it fast. This means finding sepsis early, giving the right antibiotics quickly, and following proven sepsis treatment plans.
- Implement infection control measures to prevent pneumonia, such as hand hygiene and vaccination programs.
- Employ ARDS prevention strategies, including lung-protective ventilation, to mitigate the risk of respiratory complications.
- Promptly recognize and manage sepsis to reduce the likelihood of progressing to ALI and ARDS.
| Prevention Strategies | Potential Impact |
|---|---|
| Pneumonia prevention | Reduces the risk of direct lung injury and subsequent ALI/ARDS |
| Sepsis management | Lowers the incidence of indirect lung injury and ARDS development |
| Lung-protective ventilation | Minimizes ventilator-induced lung injury and ARDS progression |
By focusing on these prevention steps and tackling risk factors, healthcare teams can greatly improve patient outcomes. This is especially true for those at risk of ALI and ARDS.
Recovery Process and Rehabilitation
Surviving acute lung injury (ALI) or acute respiratory distress syndrome (ARDS) is tough. But, the journey to recovery is key. Good rehabilitation programs help patients get stronger, breathe better, and live better lives.
Physical Rehabilitation
The path to getting better from ARDS involves many steps. Patients do exercises and therapies to boost their breathing, muscles, and health. This includes:
- Breathing exercises and lung expansion techniques
- Aerobic exercise, such as walking or stationary cycling
- Strength training to rebuild muscle mass and endurance
- Occupational therapy to regain daily living skills
- Physical therapy to improve mobility and balance
Psychological Support
Recovering from ARDS also means dealing with mental health. Patients might face:
- Anxiety and depression from their illness
- Post-traumatic stress disorder (PTSD) from their experiences
- Cognitive impairments, like memory loss or trouble focusing
Rehab programs offer counseling, support groups, and mental health help. This way, patients can handle the emotional side of recovery.
Combining physical and mental support, healthcare teams help ARDS survivors regain strength and independence. This lets them take back their lives after facing respiratory failure.
Latest Research and Treatment Advances
Recent years have seen big steps forward in studying acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). Scientists are looking into new treatments and improving old ones. This gives hope to those fighting respiratory failure.
One exciting area is extracorporeal membrane oxygenation (ECMO). It’s a method that helps by passing blood through an artificial lung. Studies show it can help in severe ARDS cases when usual breathing help doesn’t work.
Stem cell therapy is also being studied for ARDS treatment. Early findings suggest it might lessen lung inflammation and help repair tissues. This could lead to better recovery for patients.
| Recent Advancements in ARDS Research | Potential Impact |
|---|---|
| Extracorporeal Membrane Oxygenation (ECMO) | Improved management of severe ARDS cases |
| Stem Cell Therapy | Reduced lung inflammation and enhanced tissue repair |
| Novel Mechanical Ventilation Strategies | Optimized lung-protective ventilation and patient outcomes |
Researchers are also working on new ways to help with breathing. They aim to reduce damage from the ventilator and help the lungs heal. This could lead to better care for those with respiratory issues.
As we learn more about ARDS and ALI, new treatments are emerging. These could offer more effective and tailored care for those with respiratory problems.
Conclusion
In the complex world of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS), early action is crucial. We need to recognize these conditions quickly and manage them well. Ongoing research is also key to better patient care.
These severe lung problems require a team effort. We must use timely diagnosis and specific treatments. Understanding the causes is also vital.
Inflammation plays a big role in ARDS. Finding and fixing the causes is essential. Thanks to new diagnostic tools and treatments, doctors can help patients more effectively.
The future looks bright for managing ALI and ARDS. Scientists are working hard to find new solutions. Together, we can make a difference and help patients recover.
FAQ
Q: What is Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS)?
A: ALI and ARDS are severe lung conditions. They cause inflammation and fluid buildup in the lungs. This makes it hard for the lungs to exchange gases, leading to breathing failure.
Q: What are the key characteristics and diagnostic criteria of ALI and ARDS?
A: ALI and ARDS have sudden respiratory symptoms and lung X-rays show fluid. ARDS is more severe, based on how low oxygen levels get.
Q: What causes respiratory failure in ALI and ARDS?
A: Damage to the lung’s air sacs and blood vessels causes respiratory failure. This damage is often due to inflammation.
Q: What are the common causes and risk factors for ARDS?
A: ARDS can come from direct lung injuries like pneumonia or indirect injuries like sepsis. Conditions like trauma and pancreatitis also raise the risk.
Q: How are ALI and ARDS diagnosed and assessed?
A: Doctors use X-rays, CT scans, and blood tests to diagnose ALI and ARDS. They check how well the lungs are working.
Q: What is the role of inflammation in the development of ARDS?
A: Inflammation is key in ARDS. It damages the lung’s air sacs and blood vessels, leading to fluid buildup and poor gas exchange.
Q: How are ALI and ARDS treated?
A: Treatment starts with stabilizing the patient. Then, it focuses on ventilation, oxygen therapy, and treating the cause. The treatment plan is always being adjusted.
Q: What are the key strategies for mechanical ventilation in ARDS?
A: For ARDS, ventilation strategies use lower volumes and positive pressure. This helps protect the lungs and keep oxygen levels up.
Q: What are the potential complications and long-term effects of ALI and ARDS?
A: Short-term complications include respiratory failure and fluid buildup. Long-term effects can be lung damage, brain issues, and a lower quality of life.
Q: How can the risk of ALI and ARDS be reduced?
A: To prevent ALI and ARDS, treat infections and manage sepsis. Also, take steps to protect those at high risk.
Q: What does the recovery process and rehabilitation look like for ARDS survivors?
A: Survivors go through physical therapy to improve lung function and strength. They also get mental health support to deal with the condition’s effects.
Q: What are the latest research and treatment advances in ALI and ARDS?
A: Research aims to find new treatments and improve ventilation. It also looks at ways to fight inflammation and better patient outcomes.
