Did you know up to 75% of women will get vulvovaginitis, also known as leucorrhoea, at some point? This common issue causes inflammation in the vulva and vagina. It can really affect a woman’s life and health.
Vulvovaginitis includes many conditions that cause abnormal discharge, irritation, and discomfort. It’s important to know what causes it, recognize the signs, and get medical help quickly. This helps manage the condition better.

In this guide, we’ll look at different types of vulvovaginitis, their causes, and the best treatments. Whether you’re facing a yeast infection, bacterial vaginosis, or another vaginal issue, this article will help. It aims to give you the knowledge and tools to manage your reproductive health.
Key Takeaways
- Vulvovaginitis, or leucorrhoea, is a common reproductive health issue affecting up to 75% of women.
- Vulvovaginitis is characterized by inflammation of the vulva and vagina, often accompanied by abnormal vaginal discharge.
- Understanding the underlying causes, recognizing the signs and symptoms, and seeking timely medical intervention are crucial for managing vulvovaginitis.
- This article will explore the various types of vulvovaginitis, their causes, and the most effective treatment approaches.
- Addressing vulvovaginitis is essential for maintaining overall reproductive health and well-being.
Understanding Vulvovaginitis: A Comprehensive Overview
Vulvovaginitis, also known as leucorrhoea, is a common condition in women. It causes inflammation and irritation in the vulva and vagina. It also leads to abnormal vaginal discharge. This overview covers the causes, how it works, and its effects on women’s health.
Many things can cause vulvovaginal inflammation. These include reproductive tract infections, changes in vaginal pH, and sensitivity to certain products. These factors can upset the balance of the vaginal ecosystem. This can lead to an overgrowth of harmful microorganisms and vulvar irritation.
The vagina has a natural balance of beneficial bacteria, known as the vaginal microbiome. When this balance is disrupted, it can cause different types of vulvovaginitis. These include bacterial vaginosis, yeast infections, and sexually transmitted infections. Knowing the causes is key to managing and preventing it.
| Common Causes of Vulvovaginitis | Symptoms | Risk Factors |
|---|---|---|
| Bacterial vaginosis | Thin, gray, foul-smelling discharge | Antibiotic use, poor hygiene, douching |
| Candidiasis (yeast infection) | Thick, white, cottage cheese-like discharge | Diabetes, antibiotic use, pregnancy |
| Trichomoniasis | Frothy, yellow-green, foul-smelling discharge | Unprotected sexual activity, poor hygiene |
Keeping the vagina healthy is important for reproductive well-being. By knowing the causes and risk factors of vulvovaginitis, people can prevent and manage it. This helps promote long-term reproductive tract health.
Common Types of Vaginal Discharge and Their Significance
The vagina naturally makes a clear or white discharge, called leucorrhoea. This helps keep the balance of bacteria and pH levels healthy. But, if the amount, color, or texture of this discharge changes, it might mean there’s a vaginal discharge issue that needs attention.
Normal Discharge Characteristics
A healthy vaginal discharge is clear to white and has a mild smell. The amount and texture can change during the menstrual cycle. It’s more during ovulation and before your period starts.
Abnormal Discharge Signs
Abnormal vaginal discharge might look different:
- It could be thick, lumpy, or like cottage cheese.
- The color might be grey, green, yellow, or off-white.
- It might smell strong, foul, or fishy.
- You might also feel itching, burning, or irritation in the vaginal area.
When to Seek Medical Attention
If your vaginal discharge changes a lot, you should see a doctor. Abnormal discharge could mean you have a vaginal infection, like bacterial vaginosis, yeast infection, or a sexually transmitted infection. Getting a diagnosis and treatment quickly is important to keep your vagina healthy.
| Characteristic | Normal Discharge | Abnormal Discharge |
|---|---|---|
| Color | Clear to white | Grey, green, yellow, or off-white |
| Consistency | Thin, smooth | Thick, lumpy, or cottage cheese-like |
| Odor | Mild, inoffensive | Strong, foul, or fishy |
| Accompanying Symptoms | None | Itching, burning, or irritation in the vaginal area |
“Paying attention to changes in your vaginal discharge can help you identify potential health concerns and seek appropriate medical attention.”
Primary Symptoms and Signs of Vulvovaginitis
It’s important to know the main symptoms of vulvovaginitis to tackle this common vaginal health issue. Vulvovaginitis, or vaginitis, is when the vulva and vagina get inflamed. It comes with several annoying symptoms.
Vulvar irritation is a common sign. People might feel constant itching, burning, or discomfort in their external genital area. This can really bother them and make daily tasks hard.
Another symptom is changes in vaginal discharge. You might see more discharge, a different color or smell, or a weird odor. These vaginitis symptoms could mean there’s an infection or a balance problem in your vagina.
Redness and swelling in the vulva and vagina are also common. The area might look inflamed and feel sore when touched. This adds to the discomfort people feel.
“Recognizing the signs of vulvovaginal inflammation is the first step in seeking appropriate medical attention and addressing the underlying cause.”
The symptoms of vulvovaginitis can differ based on the cause. It could be bacterial vaginosis, yeast infections, or sexually transmitted infections. Getting a medical check-up is key to finding out what’s wrong and how to treat it.
Knowing the main symptoms and signs of vulvovaginitis helps you spot and deal with any vaginal health issues. This way, you can keep your overall health and quality of life in check.
Bacterial Vaginosis: Causes and Risk Factors
Bacterial vaginosis is a common vaginal infection. It happens when the balance of bacteria in the vagina gets upset. This condition is known for a bad smell and a thin, gray, or watery discharge. Knowing what causes and increases the risk of bacterial vaginosis is key to managing and preventing it.
Identifying Bacterial Vaginosis
Bacterial vaginosis is caused by too many bacteria, like Gardnerella vaginalis, in the vagina. This can happen due to douching, using scented feminine products, or having sex with many partners. Signs of bacterial vaginosis include:
- Thin, gray, or watery vaginal discharge
- A fishy or unpleasant odor
- Itching or irritation in the vagina or vulva
Prevention Strategies
To lower the risk of bacterial vaginosis, keeping your vagina healthy is important. Some ways to do this include:
- Avoiding douching or the use of scented feminine products
- Practicing good hygiene, like wiping from front to back after using the bathroom
- Limiting the number of sexual partners and using protection during intercourse
- Maintaining a healthy diet and lifestyle
Treatment Options
If you think you have bacterial vaginosis, seeing a doctor is crucial. They can diagnose it and suggest treatments. Treatments may include:
- Prescription antibiotics, such as metronidazole or clindamycin
- Over-the-counter probiotic supplements to restore vaginal flora
- Topical creams or gels to alleviate symptoms
By knowing the causes, risk factors, and treatments for bacterial vaginosis, you can keep your vagina healthy. This way, you can address any issues quickly.
Vulvovaginitis(Leucorrhoea) diseases: Clinical Manifestations
Vulvovaginitis, also known as leucorrhoea, is a common gynecological condition. It shows a wide range of symptoms. Knowing the vulvovaginitis symptoms and leucorrhoea signs is key for doctors to diagnose and treat it right.
One main vulvovaginitis symptom is abnormal vaginal discharge. This discharge can be different in color, consistency, and smell. It can be thin and watery or thick and curd-like. Patients might also feel itching, burning, or irritation in the vulvar and vaginal area.
- Thin, watery discharge may indicate a yeast infection or trichomoniasis.
- Thick, curd-like discharge is often associated with bacterial vaginosis.
- Foul-smelling discharge can be a sign of various vulvovaginal infections.
Other leucorrhoea signs include redness, swelling, and pain in the vulvar and vaginal area. Some patients might also have painful urination or painful intercourse.
“The range and severity of vulvovaginitis symptoms and leucorrhoea signs can vary greatly. It’s crucial for healthcare providers to do a thorough examination and diagnostic testing to find the underlying cause.”
In some cases, vulvovaginitis may also cause systemic symptoms like fever, chills, or pelvic pain. These symptoms suggest a more serious condition and need immediate medical attention.
By understanding the different symptoms of vulvovaginitis and leucorrhoea, healthcare providers can create the right treatment plan. This helps to ease the patient’s discomfort and treat the root cause of the condition.
Candida Infections and Their Impact on Vaginal Health
Candida infections, also known as yeast infections, are common. They can affect vaginal health a lot. These infections happen for many reasons, like hormonal changes or antibiotics. It’s key to know the types of yeast infections and how to manage them.
Types of Yeast Infections
Yeast infections come in different forms. Each has its own signs and symptoms. Here are the most common ones:
- Vulvovaginal candidiasis (VVC): This is the usual yeast infection. It causes itching, burning, and a thick, white discharge that looks like cottage cheese.
- Recurrent vulvovaginal candidiasis (RVVC): Some women get yeast infections over and over. This can be hard to deal with and might mean there’s an underlying health issue.
- Candida balanoposthitis: This infection affects the penis and foreskin. It usually happens in men who have sex with a woman who has a yeast infection.
Management Approaches
Managing candidiasis needs a full plan. It should tackle the symptoms and the root causes. Treatment might include:
- Antifungal medications: Creams or pills like azoles or fluconazole are often used first.
- Lifestyle changes: Keeping clean, wearing breathable clothes, and avoiding too much moisture can help.
- Dietary changes: Eating less sugar and refined foods can help stop Candida from growing.
- Probiotics: Taking probiotics, especially Lactobacillus, can help keep the vagina healthy and prevent infections.
Knowing about yeast infections and using a good management plan can help keep the vagina healthy. This way, you can fight candidiasis effectively.
Trichomoniasis: Transmission and Prevention
Trichomoniasis is a common sexually transmitted infection (STI) caused by a parasite called Trichomonas vaginalis. It can cause vulvovaginitis, which is inflammation of the vagina and vulva. Knowing how it spreads and how to prevent it is key to keeping vaginal health safe.
How Trichomoniasis Spreads
Trichomoniasis mainly spreads through sexual contact with an infected partner. The parasite can be passed during unprotected sex, like vaginal, oral, or anal sex. It can affect anyone, regardless of gender or sexual orientation.
Symptoms of Trichomoniasis
- Vaginal discharge that may be frothy, yellow-green, or grayish in color
- Itching, burning, redness, or soreness of the vagina and vulva
- Discomfort during urination or intercourse
- In some cases, there may be no noticeable symptoms at all
Preventing Trichomoniasis
To lower the risk of trichomoniasis and other sexually transmitted infections, safe sex is crucial. This means:
- Using condoms or other barrier methods during sexual activity
- Limiting the number of sexual partners
- Getting regularly tested for STIs, even if you don’t have symptoms
- Talking openly with sexual partners about health
If someone has trichomoniasis, it’s important their sexual partners get treated too. This stops the infection from spreading and coming back.
“Trichomoniasis is a common, curable sexually transmitted infection that can have serious consequences if left untreated. Practicing safe sex and regular STI testing are essential steps in preventing and managing this condition.”
By knowing how it spreads and taking steps to prevent trichomoniasis, you can keep your vaginal health safe. This also helps lower the risk of other sexually transmitted infections.
Diagnosing Vulvovaginal Conditions
It’s very important to accurately diagnose vulvovaginal conditions. This is because it helps in finding the right treatment. The process includes lab tests, physical exams, and ruling out other possible causes of symptoms.
Laboratory Tests
Healthcare providers use different lab tests to check for vaginal health issues. These include:
- Vaginal pH testing to check acidity levels
- Wet mount examination to find microorganisms
- Cultures or NAATs to detect pathogens like Candida or Trichomonas
- Gram stain to look at vaginal bacteria
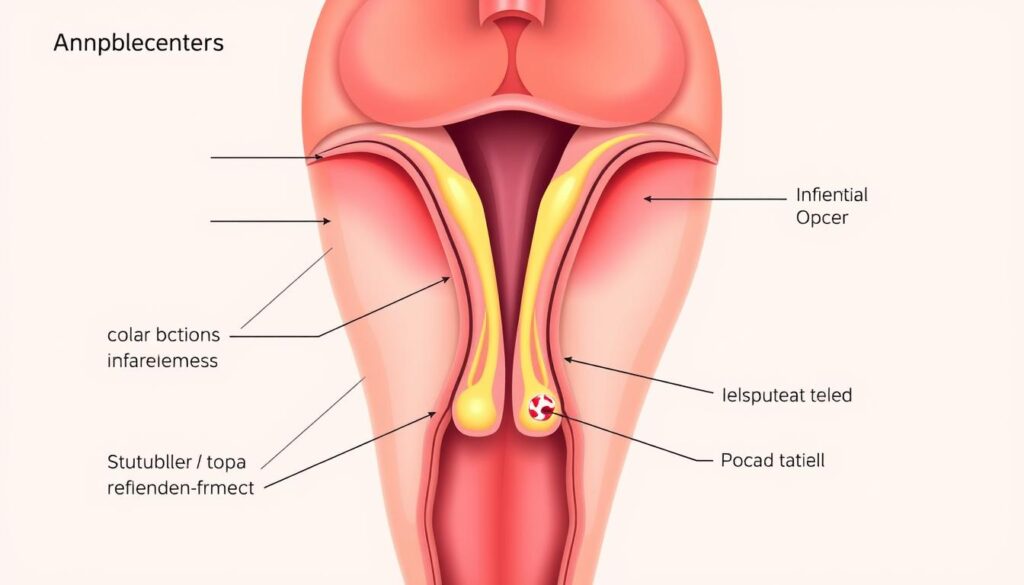
Physical Examination Process
A detailed physical exam is key in diagnosing vaginal health. The doctor will do a pelvic exam to look at the vulva, vagina, and cervix. They might use a speculum to see the vaginal walls and cervix better.
Differential Diagnosis
To find the real cause of symptoms, doctors must consider other possible conditions. This includes:
- Urinary tract infections
- Sexually transmitted infections
- Skin conditions on the vulva
- Allergic reactions or irritation
By using lab tests, physical exams, and ruling out other conditions, doctors can find the exact vaginal health diagnosis. They can then create a treatment plan for vulvovaginitis testing and the patient’s overall health.

| Laboratory Test | Purpose |
|---|---|
| Vaginal pH Testing | Check acidity levels in the vagina |
| Wet Mount Examination | Find microorganisms |
| Cultures or NAATs | Detect specific pathogens, such as Candida or Trichomonas |
| Gram Stain | Look at vaginal bacteria |
Treatment Approaches for Different Types of Vaginitis
Managing vaginitis treatment and vulvovaginitis management often involves a mix of strategies. The right plan depends on the cause of the issue. Here’s a look at the treatments for various vaginitis types:
Bacterial Vaginosis
For bacterial vaginosis, doctors usually prescribe antibiotics. These can be oral or topical, like metronidazole or clindamycin. They help balance the vaginal bacteria and ease symptoms. Probiotics and good hygiene also help prevent future infections.
Yeast Infections
Yeast infections, or vulvovaginal candidiasis, are treated with antifungal meds. These can be oral pills or creams/suppositories. Over-the-counter options like miconazole or clotrimazole work for mild cases. But, stronger or recurring infections might need prescription-strength treatments.
Trichomoniasis
Trichomoniasis, a sexually transmitted infection, is treated with a single dose of an oral antiprotozoal. This is usually metronidazole or tinidazole. It’s key for both partners to get treated to stop re-infection and spread.
Changing your lifestyle can also help manage vaginitis and vulvovaginitis. Good genital hygiene, avoiding irritants, and safe sex are important.
Working with a healthcare provider is crucial to find the best treatment. They’ll consider the type of vaginitis and your situation. Following the right treatment can help heal your vagina and prevent future problems.
Natural Remedies and Self-Care Measures
Managing vulvovaginitis, or vaginal inflammation, can be helped by natural remedies and self-care. These methods can work alongside medical treatments. They help relieve symptoms and improve vaginal health.
Dietary Modifications
Changing your diet can support vaginal health and reduce vulvovaginitis symptoms. Here are some dietary tips:
- Eat more probiotic-rich foods like yogurt, kefir, and fermented veggies. They help balance good bacteria in the vagina.
- Reduce sugary and refined carbs. They can grow bad bacteria and yeast.
- Add anti-inflammatory foods like berries, leafy greens, and fatty fish. They can lessen inflammation and discomfort.
Lifestyle Changes
Some lifestyle changes can also help vaginal health and natural remedies for vaginitis:
- Wear breathable, cotton underwear and avoid tight clothes. They trap moisture.
- Don’t douche. It can upset the vagina’s pH balance and cause irritation.
- Manage stress with yoga, meditation, or deep breathing. Stress can weaken your immune system and increase infection risk.
While these vaginal health self-care steps are helpful, see a healthcare provider if symptoms don’t get better or get worse. They can diagnose and suggest the best treatment for you.
Prevention Strategies and Hygiene Practices
Keeping your vulvovaginitis prevention and vaginal hygiene up is key for good reproductive health. Simple steps in your daily life can lower the chance of getting vaginal infections. These infections can be uncomfortable and troublesome.
Good personal hygiene is a big step in preventing vulvovaginitis. Clean the outside of your genitals with mild, fragrance-free soap and water. Then, gently pat them dry. Stay away from harsh or scented products, as they can upset the vagina’s pH balance.
- Wear breathable, cotton underwear to help keep the genital area dry and prevent the growth of harmful bacteria.
- Change out of sweaty or damp clothing as soon as possible to maintain a healthy, moisture-free environment.
- Wipe from front to back after using the restroom to prevent the spread of harmful bacteria.
Your diet and lifestyle also matter. Eating a balanced diet with lots of nutrients but less sugar helps your vagina stay healthy. Regular exercise and managing stress are also good for your vaginal health and can prevent vulvovaginitis.
| Prevention Strategies | Hygiene Practices |
|---|---|
| Wear breathable, cotton underwear | Use mild, fragrance-free soap and water |
| Change out of sweaty or damp clothing | Wipe from front to back after using the restroom |
| Consume a balanced, nutrient-rich diet | Maintain a healthy vaginal microbiome |
By following these prevention and hygiene tips, you can keep your vagina healthy. This reduces the risk of getting infections that can be uncomfortable and keep coming back.
Complications and Long-term Health Implications
Vulvovaginitis can cause serious problems if not treated or if it keeps coming back. It’s important to know these risks to get help quickly and manage it well.
Fertility Impact
Not treating vulvovaginitis can harm your ability to have children. It can cause scars and inflammation in your reproductive areas. This might make it hard to get pregnant.
Some types of vulvovaginitis, like vulvovaginal candidiasis, raise the risk of pelvic inflammatory disease. This can also hurt your chances of getting pregnant.
Chronic Conditions
Recurring or untreated vulvovaginitis can lead to chronic diseases. For example, bacterial vaginosis may increase the risk of getting sexually transmitted infections, including HIV. It can also lead to chronic pelvic pain and interstitial cystitis.
Getting a quick diagnosis and proper treatment is key to avoiding long-term problems. Regular visits to your healthcare provider and following their advice can help keep your reproductive health safe.
“Addressing vulvovaginitis early and effectively is essential for maintaining a healthy reproductive system and avoiding long-term consequences.”
When to Consult a Healthcare Provider
Getting medical help quickly is key to handling vulvovaginal issues. Some mild symptoms can be managed on your own. But, there are times when you need to see a doctor for a proper check-up and treatment.
If you notice these symptoms, it’s time to make an appointment:
- Persistent or worsening vaginal discharge with an odd smell, color, or texture
- Itching, burning, or irritation in the genital area
- Pain or discomfort during sex or other activities
- Fever, chills, or other signs of infection
- Recurring or hard-to-treat vulvovaginal infections
Seeing a doctor early is vital for treating vulvovaginitis well and avoiding complications. A healthcare provider can do a full gynecological consultation, run tests, and create a treatment plan just for you.
Also, if your menstrual cycle changes, you have chronic vulvovaginal issues, or you’re pregnant and have vaginal symptoms, see a doctor. Quick diagnosis and treatment can ease discomfort, stop infections from spreading, and keep your vagina healthy.
“Listening to your body and recognizing when something is not right is the first step in seeking the appropriate medical care for vulvovaginal concerns.”
Talking openly with your healthcare provider is crucial for dealing with vulvovaginal problems. By being proactive about your gynecological health, you can take charge of your well-being and improve your life quality.
Conclusion
Vulvovaginitis and leucorrhoea are common issues that need quick attention and the right treatment. Knowing about different types of vaginal discharge and recognizing symptoms is key. Women can manage these problems and keep their vaginal health in check by getting medical help when needed.
Managing vulvovaginitis means tackling the root causes like bacterial vaginosis, candida, or trichomoniasis. A mix of medicine, natural treatments, and changes in lifestyle can help. This approach can ease discomfort, stop it from coming back, and protect vaginal and reproductive health for the long term.
It’s important to focus on vaginal health awareness. Learning about vaginal health, keeping clean, and watching for any changes in discharge are essential. By doing this, women can play a big role in managing their vulvovaginitis and overall health. Getting medical help quickly is key to getting the right treatment and taking back control of vaginal health.
FAQ
Q: What is vulvovaginitis(leucorrhoea)?
A: Vulvovaginitis, also known as leucorrhoea, is a condition. It causes inflammation of the vulva and vagina. It often comes with abnormal vaginal discharge.
Q: What are the main causes of vulvovaginitis?
A: Vulvovaginitis can be caused by several things. Bacterial infections, like bacterial vaginosis, are common. Fungal infections, such as candidiasis, are also a cause. Sexually transmitted infections, like trichomoniasis, and irritation from chemicals or allergens can also cause it.
Q: What are the common symptoms of vulvovaginitis?
A: Symptoms of vulvovaginitis include itching and burning. You might also see redness and changes in vaginal discharge. This can include more discharge, different color, or a bad smell.
Q: How is vulvovaginitis diagnosed?
A: Doctors diagnose vulvovaginitis by looking at your medical history and doing a physical exam. They might also do tests like looking at vaginal secretions under a microscope or cultures to find the cause.
Q: What are the treatment options for vulvovaginitis?
A: Treatment for vulvovaginitis depends on the cause. It might include antibiotics, antifungal meds, or topical treatments. Changing your lifestyle, like improving hygiene and diet, might also be suggested.
Q: How can vulvovaginitis be prevented?
A: To prevent vulvovaginitis, keep your genital area clean. Wear breathable underwear and avoid douching. Safe sex practices are also key. Regular check-ups with a doctor can help catch and treat any issues early.
Q: When should someone seek medical attention for vulvovaginitis?
A: See a doctor if your symptoms get worse or don’t get better with self-care. This includes severe itching, burning, or changes in discharge. Early treatment is crucial for your vaginal health.
Q: Can vulvovaginitis affect fertility or lead to long-term health issues?
A: Yes, untreated vulvovaginitis can affect fertility. It can also lead to chronic conditions. Working closely with a healthcare provider is key to managing it and preventing long-term problems.
Q: What are some natural remedies and self-care measures for managing vulvovaginitis?
A: Natural remedies and self-care can help manage vulvovaginitis. Dietary changes, probiotics, breathable clothing, and good hygiene are some options. But, always talk to a healthcare provider before trying new treatments.
