Did you know nearly one in five adults in the United States has chronic dry mouth? This condition, known as xerostomia, affects oral health and overall well-being. It’s important to understand the causes and find effective treatments.
Xerostomia, or dry mouth, means you don’t have enough saliva. This makes your mouth feel dry and uncomfortable. This article will explore why it happens, its effects on daily life, and how to treat it.

Key Takeaways
- Xerostomia, or dry mouth, is a surprisingly common condition affecting nearly 20% of adults in the United States.
- Saliva plays a crucial role in maintaining oral health, and a lack of saliva production can lead to a range of problems.
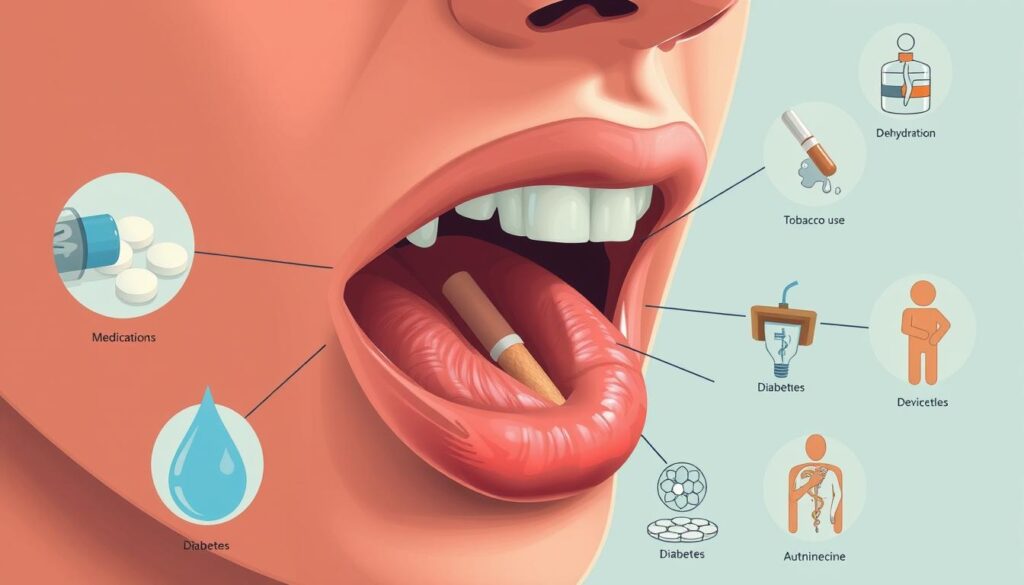
- Numerous medical conditions, medications, and lifestyle factors can contribute to the development of xerostomia.
- Dry mouth can have a significant impact on daily life, including difficulties with speaking, eating, and swallowing.
- Effective treatment options for xerostomia include prescription medications, artificial saliva products, and lifestyle modifications.
Understanding Xerostomia(Dry mouth): An Overview
Xerostomia, or dry mouth, is a common issue that affects how much saliva we make. Saliva is key for keeping our mouths healthy. It helps us digest food and protects our teeth and gums from harm.
The Role of Saliva in Oral Health
Saliva is more than just water in our mouths. It’s a mix of water, enzymes, proteins, and antibodies. It helps us chew and swallow food. It also breaks down food and protects our teeth from acid damage.
Impact on Daily Life and Well-being
When we don’t make enough saliva, it can really affect our lives. Dry mouth makes it hard to speak, swallow, and taste food. It also raises the risk of tooth decay and gum disease.
Dry mouth can make everyday activities harder. It can hurt our enjoyment of meals and social events. Knowing how important saliva is helps us find ways to manage dry mouth and keep our mouths healthy.
Common Signs and Symptoms of Dry Mouth
Feeling dry mouth symptoms, or xerostomia, can be really frustrating. It happens when you don’t have enough saliva. This can cause a lot of problems that affect your mouth and overall health.
Here are some common signs and symptoms of oral dryness:
- Persistent thirst and the constant need to sip water or other liquids
- Difficulty swallowing dry foods or experiencing a burning sensation in the mouth
- Changes in taste perception, with foods tasting different or less flavorful
- Frequent dental cavities, gum disease, or other oral health problems
- Irritation, redness, or a feeling of stickiness or stringiness in the mouth
- Difficulty speaking or a hoarse, rough voice
If you notice any of these dry mouth symptoms, see a healthcare professional. They can find out why you have it and help you get better. Treating xerostomia can make you feel better, improve your mouth health, and make life better overall.
“Dry mouth is more than just an inconvenience – it can lead to serious dental and health problems if left untreated.”
The Science Behind Saliva Production
Saliva is key to keeping our mouths healthy. Knowing how it’s made is important. This part talks about the glands that make saliva and how it’s secreted. It helps us understand problems like xerostomia (dry mouth).
Anatomy of Salivary Glands
We have three main pairs of salivary glands: parotid, submandibular, and sublingual. They’re around our mouth and make most of our saliva. Inside these glands, special cells make saliva. It then goes through ducts to our mouth.
Normal Saliva Production Processes
Making saliva is complex. It involves many steps. When we see, smell, or taste food, it starts. This sends signals to our glands. They then make saliva, which is mostly water, salts, and proteins.
Factors Affecting Salivary Flow
- Age: As we get older, our glands make less saliva.
- Medications: Some drugs can mess with our glands, causing dry mouth.
- Medical Conditions: Diseases, radiation, and some brain issues can affect saliva.
- Lifestyle Factors: Not drinking enough water, being stressed, or smoking can also lower saliva.
Knowing how saliva is made helps us find and fix problems like xerostomia. It’s key for good oral health.
Medical Conditions Leading to Xerostomia
Dry mouth, or xerostomia, can be caused by many medical conditions. Sjogren’s syndrome is a common one. It’s an autoimmune disorder that attacks the glands that make moisture, leading to less saliva.
Diabetes can also cause dry mouth by affecting the salivary glands. People with uncontrolled diabetes often have salivary gland dysfunction. This makes dry mouth symptoms worse.
Radiation therapy for head and neck cancers is another big cause. The radiation can harm the salivary glands. This can greatly reduce saliva flow, affecting oral health and overall well-being.
| Medical Condition | Mechanism of Dry Mouth |
|---|---|
| Sjogren’s Syndrome | Autoimmune attack on moisture-producing glands |
| Diabetes | Salivary gland dysfunction |
| Radiation Therapy for Head and Neck Cancers | Damage to salivary glands |
It’s important to know the medical conditions that cause dry mouth. This helps in finding the right treatment. Healthcare providers can then create plans to help manage xerostomia.
“Addressing the underlying medical condition is the key to managing xerostomia effectively.”
Medications That Can Cause Dry Mouth
Dry mouth, or xerostomia, is a common side effect of some medications. Both prescription and over-the-counter drugs can lead to this issue. It’s important to know which medications can cause dry mouth to manage it better.
Prescription Medications
Many prescription drugs can cause dry mouth. These xerogenic medications include antidepressants, antihistamines, and pain relievers. Taking these can reduce saliva, making your mouth feel dry.
Over-the-Counter Drugs
Some over-the-counter (OTC) medications can also cause dry mouth. Antihistamines and pain relievers without a prescription can have similar effects. People using these should watch out for medication side effects on their mouth.
Treatment Alternatives
If medication causes dry mouth, there are other ways to help. You might need to switch medications or change the dosage. Using artificial saliva or chewing sugar-free gum can also help.
Good oral hygiene and staying hydrated are key to managing dry mouth. Knowing the causes and finding solutions can help keep your mouth healthy.
Lifestyle Factors Contributing to Oral Dryness
Keeping your mouth healthy is more than just managing health issues. Some lifestyle choices can make dry mouth worse. Knowing these lifestyle factors helps tackle dry mouth causes and manage xerostomia risk factors.
Smoking is a big lifestyle factor for dry mouth. It harms the salivary glands, reducing saliva. Alcohol consumption also dries out the mouth by making it hard to stay hydrated.
- Not drinking enough water or using too many diuretics can lead to dry mouth causes.
- Eating too much salt or sugar can worsen xerostomia risk factors by upsetting the mouth’s balance.
Our lifestyle choices greatly affect our mouth’s health. By tackling these lifestyle factors, we can fight dry mouth causes and boost our oral health.
Complications and Associated Health Risks
Chronic dry mouth, or xerostomia, can cause many problems. These issues can harm your oral health and overall health. It’s important to know about these risks if you have this condition.
Dental Problems
One big worry with xerostomia is dental problems. Saliva helps keep your mouth healthy by neutralizing acids and cleaning away food. Without enough saliva, your teeth and gums are more at risk for decay and disease.
Oral Infections
Dry mouth also raises the chance of oral infections. For example, candidiasis (thrush) can cause painful sores. Without enough saliva, your mouth can’t fight off infections as well.
Quality of Life Impact
Xerostomia can affect more than just your mouth. It can make it hard to swallow, speak, and enjoy food. This can make you feel uncomfortable in social situations and lower your overall happiness.
| Xerostomia Complication | Description | Potential Impact |
|---|---|---|
| Dental Problems | Increased risk of tooth decay, gum disease, and other dental issues due to reduced saliva production. | Tooth loss, pain, and expensive dental treatments. |
| Oral Infections | Increased risk of fungal infections, such as candidiasis (thrush), due to an imbalance of oral microorganisms. | Painful sores, irritation, and difficulty eating or speaking. |
| Quality of Life Impact | Difficulty with swallowing, speaking, and enjoying meals, leading to social discomfort and decreased sense of well-being. | Impaired social interactions, sleep problems, and reduced overall enjoyment of daily activities. |
It’s key to know the risks of xerostomia. By understanding these risks and getting the right treatment, you can protect your oral health and improve your life quality.
Diagnostic Approaches for Xerostomia
Diagnosing dry mouth, or xerostomia, is key to finding the right treatment. Doctors use different methods to find out why and how severe it is.
The salivary flow rate test is a main tool. It measures saliva over time. This shows if someone’s saliva is normal or if it’s low, meaning they have dry mouth.
Doctors also look at a patient’s medical history. This helps find out if other health issues, medicines, or habits might be causing dry mouth.
- A detailed check of the mouth, tongue, gums, and glands gives clues about oral health and how bad the dry mouth is.
- Sialometry measures saliva from the glands, at rest and when stimulated, to check flow.
- Sialochemistry analyzes saliva’s chemical makeup to spot any issues that might lead to dry mouth.
| Diagnostic Approach | Purpose |
|---|---|
| Salivary Flow Rate Test | Measure the amount of saliva produced to determine if it is within normal range |
| Medical History Evaluation | Identify underlying medical conditions, medications, or lifestyle factors contributing to dry mouth |
| Comprehensive Oral Examination | Inspect the mouth, tongue, gums, and salivary glands to assess the severity of xerostomia |
| Sialometry | Precisely measure the amount of saliva produced by the salivary glands |
| Sialochemistry | Analyze the chemical composition of the patient’s saliva to identify imbalances |
Using these diagnostic approaches, doctors can find the real cause of dry mouth. They then create a treatment plan that fits the patient’s needs. This detailed check helps manage dry mouth and its problems well.

Medical Treatment Options
For those dealing with xerostomia, or dry mouth, there are many medical treatments. These aim to ease symptoms and find the root cause of this common issue.
Prescription Medications
Some prescription drugs help make more saliva. These dry mouth treatments work by getting the salivary glands to make more. Pilocarpine and cevimeline are two common ones that help a lot.
Artificial Saliva Products
When gland stimulation doesn’t work, artificial saliva products are a good choice. These xerostomia medications act like real saliva. They help keep the mouth moist and hydrated.
These products come in sprays, gels, lozenges, or mouth rinses. This lets people pick what works best for them. They help with speaking, swallowing, tasting, and prevent infections.
“Addressing the underlying causes and incorporating both medical and self-care treatments can significantly improve the quality of life for individuals suffering from dry mouth.”
Natural Remedies and Self-Care Measures
Managing dry mouth, or xerostomia, can be done with natural remedies and self-care. Drinking plenty of water is key. It helps keep your mouth moist and stimulates saliva production.
Chewing sugar-free gum or sucking on sugar-free candies also helps. They stimulate your salivary glands, providing temporary relief. Avoiding caffeine, alcohol, and spicy foods can also reduce discomfort.
Herbal remedies like green tea or licorice root can help stimulate saliva. Essential oils, like peppermint or lemon, can also offer relief when applied to the mouth and gums.
Good oral hygiene is crucial. Brush, floss, and use non-irritating toothpaste and mouthwash regularly. These steps, along with natural remedies, can help manage dry mouth and keep your mouth healthy.
| Natural Dry Mouth Remedies | Benefits |
|---|---|
| Drinking Water | Helps stimulate saliva production and keep the mouth moist |
| Chewing Sugar-Free Gum | Stimulates the salivary glands and increases saliva flow |
| Using Herbal Remedies (e.g., green tea, licorice root) | May possess properties that can help stimulate saliva production |
| Applying Essential Oils (e.g., peppermint, lemon) | May provide relief when applied topically to the mouth and gums |
| Maintaining Good Oral Hygiene | Helps manage dry mouth and maintain optimal oral health |
By using these natural remedies and self-care steps, you can manage dry mouth. This helps keep your mouth healthy and comfortable.
Prevention Strategies and Lifestyle Changes
Good oral health habits are key to preventing and managing dry mouth. By taking proactive steps, you can control your oral health. This helps reduce the effects of dry mouth on your daily life.
Dietary Modifications
Changing your diet is a crucial step in preventing dry mouth. Stay away from acidic, sugary, or spicy foods and drinks. These can dry out your mouth. Instead, eat foods that help keep your mouth moist, like:
- Water-rich fruits and vegetables (e.g., melons, cucumbers, celery)
- Dairy products (e.g., milk, yogurt, cheese)
- Whole grains (e.g., oats, brown rice, quinoa)
- Lean proteins (e.g., poultry, fish, legumes)
Oral Hygiene Practices
Keeping up with a good oral hygiene routine is vital for dry mouth prevention and xerostomia management. This includes:
- Brushing your teeth twice a day with a soft-bristled toothbrush and fluoride toothpaste
- Flossing every day to remove plaque and food
- Using an alcohol-free, non-foaming mouthwash to keep your mouth moist
- Applying a thin layer of over-the-counter saliva substitutes or lubricants as needed
By following these oral health habits daily, you can keep your mouth healthy and moist. This reduces the risks of xerostomia.
When to Seek Professional Help
Minor dry mouth can be handled with simple care. But, some cases need a healthcare expert for xerostomia treatment. If your dry mouth is persistent or severe, see a dry mouth specialist or oral health professional.
Here are signs you should see a doctor:
- Dry mouth that makes it hard to speak, swallow, or eat
- Long-lasting dry mouth that doesn’t go away
- Sudden, severe dry mouth with other worrying symptoms
- Dry mouth that causes frequent oral infections or dental issues
- Dry mouth that really affects your daily life
A dry mouth specialist or oral health professional will check you thoroughly. They’ll find the cause of your dry mouth and plan a treatment. This might include medicine, changes in your lifestyle, or other treatments to help your mouth.
| Specialist | Expertise |
|---|---|
| Dentist | Diagnose and treat dental-related causes of dry mouth, such as xerostomia due to medications or medical conditions |
| ENT (Ear, Nose, and Throat) Doctor | Evaluate and treat salivary gland disorders and other underlying medical conditions that can lead to dry mouth |
| Rheumatologist | Manage dry mouth associated with autoimmune disorders like Sjögren’s syndrome |
| Oncologist | Treat dry mouth caused by cancer treatments, such as radiation therapy or chemotherapy |
Getting professional help can help you understand your dry mouth better. You’ll get treatments that fit you, improving your mouth health and overall well-being.
Conclusion
In this guide, we’ve explored the complex world of xerostomia, or dry mouth. We’ve looked at its causes, symptoms, and how it affects oral health and overall well-being. We’ve covered the crucial role of saliva and how medical conditions and medications can lead to dry mouth.
We’ve stressed the need for xerostomia management. The article has discussed diagnostic methods, medical treatments, and the benefits of natural remedies and self-care. By increasing dry mouth awareness, we aim to help readers protect their oral health and seek help when needed.
It’s vital to understand the importance of oral health. Untreated xerostomia can have serious effects beyond the mouth, affecting quality of life. By knowing the causes, symptoms, and solutions, people can improve their oral health. This leads to better dental health and overall well-being.
FAQ
Q: What is xerostomia (dry mouth)?
A: Xerostomia, or dry mouth, is when you don’t make enough saliva. This makes your mouth feel dry all the time.
Q: What are the main causes of dry mouth?
A: Dry mouth can happen for many reasons. It might be due to health issues like Sjogren’s syndrome or diabetes. It can also be caused by medicines, radiation therapy, or habits like smoking.
Q: What are the common symptoms of xerostomia?
A: Signs of dry mouth include always feeling thirsty and trouble swallowing. You might also notice changes in taste, mouth sores, or a burning feeling in your mouth.
Q: How does saliva production work?
A: Saliva comes from glands in your mouth and throat. Dehydration, gland problems, or certain medicines can mess with how much saliva you make.
Q: What medical conditions can lead to dry mouth?
A: Health issues like Sjogren’s syndrome, diabetes, and radiation therapy can affect your salivary glands. This can lead to dry mouth.
Q: Which medications can cause dry mouth?
A: Many medicines, including antidepressants, antihistamines, and blood pressure meds, can dry out your mouth.
Q: How can lifestyle factors contribute to oral dryness?
A: Smoking, drinking too much alcohol, and not drinking enough water can all make your mouth dry. They reduce saliva or cause you to lose more water.
Q: What are the potential complications of untreated xerostomia?
A: If you don’t treat dry mouth, you might get cavities or gum disease. You could also get infections or feel less happy with your life.
Q: How is xerostomia diagnosed?
A: Doctors might do tests to see how much saliva you make. They’ll also look at your medical history to figure out if you have dry mouth.
Q: What medical treatments are available for dry mouth?
A: Doctors might prescribe medicines to help you make more saliva. They might also suggest artificial saliva or treating any health issues that cause dry mouth.
Q: What are some natural remedies and self-care measures for managing dry mouth?
A: Drinking plenty of water, chewing sugar-free gum, and avoiding foods that dry out your mouth can help. Keeping your mouth clean is also important.
Q: How can dry mouth be prevented?
A: To prevent dry mouth, eat right, brush and floss well, and manage any health issues or medicine side effects that might cause it.
Q: When should someone seek professional help for dry mouth?
A: If your dry mouth is a big problem or makes it hard to do everyday things, see a doctor. They can help figure out what’s wrong and how to fix it.
